Discover Audio Journal of Oncology Podcast
Audio Journal of Oncology Podcast

Audio Journal of Oncology Podcast
Author: Audio Medica News
Subscribed: 21Played: 118Subscribe
Share
Description
As the leading authoritative, peer-reviewed audio source of oncology clinical news for clinicians and healthcare professionals, the AJO Podcast regularly brings you exclusive interviews with the world's leading researchers and clinicians responsible for pushing out the boundaries of science and practice.
Medicine, screening, radiotherapy, surgery, clinical trials, cancer care, epidemiology and prevention are covered impartially to give busy cancer professionals access to conversational spoken comments on the clinical implications of cancer developments in the real-world context, as practiced by cancer doctors and clinicians around the globe.
The AJO Podcast originates from the Audio Journal of Oncology staffed by ex-BBC professional journalists, and mentored by world-leading cancer practitioners from bodies including the American Society of Clinical Oncology, Cancer Research UK, Istituto Nazionale dei Tumori, and Action Radiotherapy.
Each podcast is produced to the highest standards of audio recording and journalism and is subject to editorial appraisal to maintain that content, balance and clinical relevance of news and comment are delivered in a manner that's easy and enjoyable for listening while travelling, taking exercise, working or just relaxing.
Please contact Audio Medica with your comments and make your contribution to supporting a vibrant community of clinical cancer communicators!
Medicine, screening, radiotherapy, surgery, clinical trials, cancer care, epidemiology and prevention are covered impartially to give busy cancer professionals access to conversational spoken comments on the clinical implications of cancer developments in the real-world context, as practiced by cancer doctors and clinicians around the globe.
The AJO Podcast originates from the Audio Journal of Oncology staffed by ex-BBC professional journalists, and mentored by world-leading cancer practitioners from bodies including the American Society of Clinical Oncology, Cancer Research UK, Istituto Nazionale dei Tumori, and Action Radiotherapy.
Each podcast is produced to the highest standards of audio recording and journalism and is subject to editorial appraisal to maintain that content, balance and clinical relevance of news and comment are delivered in a manner that's easy and enjoyable for listening while travelling, taking exercise, working or just relaxing.
Please contact Audio Medica with your comments and make your contribution to supporting a vibrant community of clinical cancer communicators!
138 Episodes
Reverse
2025 San Antonio Breast Cancer Symposium: Selective Estrogen Degrader Giredestrant Improves on Standard Endocrine Therapy for Patients with ER-positive, HER2-negative Early Breast Cancer: Phase III lidERA Breast Cancer trial Findings
An interview with: Aditya Bardia MD MPH, Professor of Medicine and Director of Translational Research Integration, University of California, Los Angeles and Jonsson Comprehensive Cancer Center, Los Angeles, California USA.
SAN ANTONIO, USA—Significant and clinically meaningful improvements in disease-free survival were reported from the Phase III lidERA Breast Cancer trial at the 2025 San Antonio Breast Cancer Symposium, in San Antonio, USA. First author of the study, Aditya Bardia MD MPH, Professor of Medicine and Director of Translational Research Integration at University of California, Los Angeles and the Jonsson Comprehensive Cancer Center, in Los Angeles, California, met up with Audio Journal Oncology reporter, Peter Goodwin.
Audio Journal of Oncology with: Aditya Bardia MD MPH
IN “[GOODWIN] I am at the San Antonio ……. OUT: …….of Oncology. I’m Peter Goodwin” 7:42 secs
San Antonio Breast Cancer Symposium ABSTRACT: GS1-10
“Giredestrant vs standard-of-care endocrine therapy as adjuvant treatment for patients with estrogen receptor-positive, HER2-negative early breast cancer: Results from the global Phase III lidERA Breast Cancer trial
Speaker:
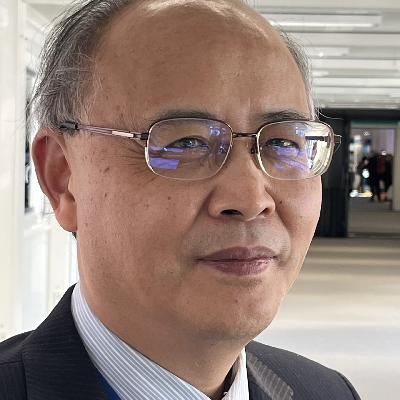
Aditya Bardia, University of California Los Angeles, Los Angeles, CA
Authors:
Bardia1, P. Schmid2, M. Martín3, S. Hurvitz4, K. Jung5, M. Rimawi6, S. Saji7, G. Werutsky8, N. Harbeck9, S. Loi10, A. Ogiya11, M. Ruiz-Borrego12, A. Alacacıoğlu13, J. Wu14, C. Ye15, M. Liste-Hermoso16, N. Withana16, T. Badovinac Crnjevic17, M. Shah18, P. Pérez-Moreno19, C. Geyer, Jr.20; 1University of California Los Angeles, Los Angeles, CA, 2Centre for Experimental Cancer Medicine, Barts Cancer Institute, Queen Mary University of London, London, UNITED KINGDOM, 3Universidad Complutense, GEICAM, CIBERONC, Madrid, SPAIN, 4Department of Medicine, UW Medicine, Fred Hutchinson Cancer Center, Seattle, WA, 5Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, KOREA, REPUBLIC OF, 6Dan L Duncan Comprehensive Cancer Center, Baylor College of Medicine, Houston, TX, 7Department of Medical Oncology, Fukushima Medical University, Fukushima, JAPAN, 8Breast Cancer Program, Latin American Cooperative Oncology Group and Centro de Pesquisa em Oncologia, Hospital Sao Lucas PUCRS, Porto Alegre, JAPAN, 9Department of Obstetrics and Gynecology, LMU University Hospital, Munich, GERMANY, 10Division of Cancer Research, Peter MacCallum Cancer Centre and The Sir Peter MacCallum Department of Oncology, University of Melbourne, Melbourne, AUSTRALIA, 11Cancer Institute Hospital, Japanese Foundation for Cancer Research, Tokyo, JAPAN, 12Breast Cancer Unit, Hospital Universitario Virgen del Rocío, Sevilla, SPAIN, 13Department of Oncology, İzmir Kâtip Çelebi University, Atatürk Training and Research Hospital, İzmir, TURKEY, 14Department of Breast Surgery, Cancer Hospital/Institute, Fudan University, Shanghai, CHINA, 15Department of Oncology Biostatistics, Genentech, Inc., South San Francisco, CA, 16Global Product Development – Clinical Science Oncology (PDOH), F. Hoffmann-La Roche Ltd, Basel, SWITZERLAND, 17PDO – Clinical Science Oncology, F. Hoffmann-La Roche Ltd, Basel, SWITZERLAND, 18Product Development Safety, Genentech, Inc., South San Francisco, CA, 19Product Development Oncology/Hematology (PDOH), Genentech, Inc., South San Francisco, CA, 20Department of Medicine, University of Pittsburgh School of Medicine-UPMC Hillman Cancer Center, Pittsburgh, PA.
Background:
Adjuvant (adj) endocrine therapy (ET) is the mainstay treatment (tx) for estrogen receptor-positive, HER2-negative early breast cancer (ER+ HER2- eBC). However, up to 1/3 of patients (pts) eventually experience recurrence. Clinically, there is an unmet need for more tolerable and efficacious ET to improve adherence and pt outcomes. Giredestrant, a next-generation oral selective estrogen receptor antagonist and degrader (SERD), was shown to be more potent than other SERDs (Liang 2021; Bardia 2023) and demonstrated superior antiproliferative activity vs anastrozole in the neoadj coopERA BC trial (Hurvitz 2023). Results of the prespecified interim analysis of the global, randomized lidERA BC trial (NCT04961996) are presented.
Methods: Pts with Stage I-III ER+ HER2- eBC were randomized 1:1 to giredestrant 30 mg oral daily (with an LHRH agonist in pre- and peri-menopausal women, and men) or standard-of-care ET (tamoxifen or aromatase inhibitor) for 5 years (yr). The primary endpoint was invasive disease-free survival (IDFS). Key secondary endpoints were overall survival (OS), distant recurrence-free interval (DRFI), and safety.
Results: 4170 pts were randomized (Aug 2021-Sep 2023): 2084 to giredestrant; 2086 to standard-of-care ET. Median age was 54.0 yr; 59.3% of pts were postmenopausal; 13.0%, 47.4%, and 39.6% had Stage I, II, and III BC, respectively. Median follow-up at clinical cutoff (Aug 8, 2025) was 32.3 months, with 336 IDFS events. Efficacy is shown in the table. Giredestrant demonstrated superior IDFS vs standard-of-care ET (hazard ratio [HR] 0.70; 95% confidence interval [CI], 0.57, 0.87; p = 0.0014). 3-yr IDFS rates were 92.4% and 89.6%, respectively. There was a trend towards OS improvement in the giredestrant arm vs the standard-of-care ET arm (HR 0.79; 95% CI, 0.56,1.12). The DRFI HR was 0.69 (95% CI, 0.54, 0.89). The most common adverse events (AEs) in the giredestrant vs standard-of-care ET arms, respectively, were arthralgia (48.0% vs 47.1%), hot flush (27.4% vs 28.8%), and headache (15.3% vs 13.2%); the most common Grade 3-4 AEs, hypertension (2.6% vs 2.0%) and arthralgia (1.5% vs 1.8%). Discontinuations due to AEs occurred in 5.3% with giredestrant vs 8.2% with standard-of-care ET.
Conclusions: lidERA BC is the first Phase III trial to demonstrate benefit with an oral SERD in eBC. Giredestrant tx resulted in a statistically significant and clinically meaningful IDFS improvement vs standard-of-care ET in ER+, HER2- eBC. OS trended in favor of the giredestrant arm, and DRFI was improved vs standard-of-care ET. The safety profile was favorable and consistent with known profiles, and the discontinuation rate was slightly lower with giredestrant compared with standard-of-care ET. Overall, the results support giredestrant as a potential new standard for pts with HR+ eBC.
PRESS RELEASE:
Novel Endocrine Therapy Giredestrant Improves Disease-free Survival Over Standard of Care for Patients With Early-stage Breast Cancer in Phase III lidERA Trial
SAN ANTONIO – The investigational, oral selective estrogen receptor degrader (SERD) giredestrant given as an adjuvant therapy showed significant improvement in invasive disease-free survival (iDFS) compared with the current standard-of-care endocrine therapy in patients with early-stage, hormone receptor (HR)-positive, HER2-negative breast cancer, according to the results of the phase III IidERA trial presented at the San Antonio Breast Cancer Symposium (SABCS), held December 9-12, 2025.
“For patients with HR-positive breast cancer—which accounts for about 70% of breast cancer cases— effective adjuvant therapy at the early stage offers a real opportunity to eradicate micrometastatic disease and improve survival in the curative setting,” said presenter Aditya Bardia, MD, MPH, professor of medicine and director of translational research integration at the University of California, Los Angeles Jonsson Comprehensive Cancer Center. “Currently, up to a third of these patients eventually experience recurrence on or after adjuvant endocrine therapy for early breast cancer, and many struggle with tolerating treatment. A more effective, more tolerable treatment option is needed.”
In the global, randomized, open-label, multicenter trial, Bardia and colleagues enrolled patients with HR- positive, HER2-negative breast cancer in stages 1-3 to evaluate the safety and efficacy of giredestrant compared with the current standard-of-care therapies. All patients enrolled had received surgery and, if indicated, completed adjuvant or neoadjuvant chemotherapy. The median age of participants was 54, and 59% were postmenopausal.
In the randomized clinical trial, the researchers assigned 4,170 patients 1:1 to receive either 30 mg of giredestrant or one of four standard-of-care endocrine therapies selected at the discretion of the prescribing physician: tamoxifen, letrozole, anastrozole, or exemestane. Patients received their treatment daily for every 28-day cycle until five years had passed or unacceptable toxicity had occurred.
The researchers assessed patients for the primary endpoint of iDFS, and secondary endpoints included overall survival (OS) and distant recurrence-free interval (DRFI).
The trial met its primary endpoint at a prespecified interim analysis. After a median follow-up of 32.3 months, patients who received giredestrant had significantly better iDFS than their counterparts who received standard-of-care endocrine therapy and were 30% less likely to develop invasive disease progression at the time of follow-up.
The secondary endpoint of DRFI was also met. Patients who received giredestrant were 31% less likely than those in the standard-of-care arm to experience distant recurrence at the time of follow-up.
“Giredestrant demonstrated clinically meaningful superiority to currently well-established standard-of-care endocrine agents: aromatase inhibitors and tamoxifen,” Bardia said. “What is particularly striking and relevant is early separation of curves,” he added, referring to the preliminary OS data. Due to the limited follow-up window, the OS data were immature but showed a positive trend in favor of giredestrant over the standard of care, he explained.
The most common treatment-emergent adverse events (TEAEs) in both the giredestrant and stand
ASH 2025 Orlando: Childhood Leukemia Cured But Families Broke. “Financial Toxicity” is Often More Worrying than you Child’s Cancer
An interview with: Daniel Zheng, Instructor, Children’s Hospital of Philadelphia, Attending Oncologist, Division of Oncology, Philadelphia PA, United States
ORLANDO, USA—Although most children with acute lymphoblastic leukemia can look forward to a cure, their families may face catastrophic financial hardship, according to Daniel Zheng, an Instructor and Attending Oncologist at the Division of Oncology, Children’s Hospital of Philadelphia in Philadelphia, PA, United States. After reporting on the challenge families face of “financial toxicity” from extended curative treatment for ALL Dr. Zheng talked about his findings from the Dana Farber Cancer Institute ALL 16-001 Trial with Audio Journal of Oncology correspondent, Peter Goodwin:
Audio Journal of Oncology: Daniel Zheng
IN: “[GOODWIN] I’m reporting direct … OUT: Oncology, I’m Peter Goodwin 7:38secs
American Society of Hematology 2025 Annual Meeting Abstract 710:
“Cumulative incidence of household material hardship and income loss as measures of financial toxicity during pediatric acute lymphoblastic leukemia (ALL) treatment: A report from the DFCI: ALL 16-001 Trial”
Authors
Daniel Zheng1, Eva Robinson 2, Yael Flamand, 3, Rahela Aziz-Bose 4, Victoria Koch3, Peter Cole5, Lisa Gennarini6, Kelly Getz7, Justine Kahn8, Kristine Karvonen9, Colleen Kelly10, Kara Kelly11, Bruno Michon12, Haley Newman1, Morgan Paul13, Thai Tran14, Puja Umaretiya15, Jennifer Welch16, Edie Weller2, 17, Lewis Silverman8, Kira Bona 10
1 Children’s Hospital of Philadelphia, Division of Oncology, Philadelphia, PA, United States,
2 Boston Children’s Hospital, Biostatistics and Research Design Center, Boston, MA, United States,
3 Dana-Farber Cancer Institute, Boston, MA, United States,
4 Dana-Farber Cancer Institute, Department of Pediatric Oncology, MD, MPH, MA, United States,
5 Rutgers Cancer Institute, New Brunswick, NJ, United States,
6 Montefiore Medical Center, Bronx, NY, United States, 7 University of Pennsylvania, Department of Epidemiology, Philadelphia, PA, United States, 8 Columbia University Irving Medical Center, Division of Pediatric Hematology, Oncology and Stem Cell Transplantation, New York, NY, United States,
9 Seattle Children’s Hospital, Division of Pediatric Hematology-Oncology, Seattle, WA, United States,
10 DanaFarber Cancer Institute, Department of Pediatric Oncology, Boston, MA, United States,
11 Roswell Park Comprehensive Cancer Center, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, Department of Pediatrics, Buffalo, NY, United States,
12 Centre Hospitalier Universitaire de Quebec, SaintFoy, QC, Canada,
13 Dana-Farber Cancer Institute, Department of Data Science, Boston, MA, United
States,
14 Charles-Bruneau Cancer Center, CHU Ste-Justine, University of Montreal, Division of Pediatric Hematology-Oncology, Montreal, QC, Canada,
15 UT Southwestern Medical Center, Department of Pediatrics, Dallas, TX, United States,
16 Hasbro Children’s Hospital/Brown University, Division of Pediatric Hematology Oncology, Providence, RI, United States,
17 Harvard Medical School, Department of Pediatrics, Boston, MA, United States
Abstract Body, Introduction:
Over 90% of children with acute lymphoblastic leukemia (ALL) will survive their cancer in the context of >2 years of multi-agent chemotherapy. This intensive treatment paradigm may lead to significant treatment-related financial toxicity for families— an outcome highly relevant to long-term child and family well-being. The magnitude and trajectories of financial toxicity are unknown in pediatric oncology, and necessary to inform optimal screening and intervention strategies for children with cancer and their families. Development of new household material hardship ([HMH], housing, food, or utility insecurity) or income loss during cancer treatment are concrete, targetable metrics of financial toxicity.
We present results from Dana-Farber Cancer Institute (DFCI) ALL Consortium Trial 16-001, the first pediatric oncology clinical trial to systematically collect longitudinal HMH and household income data as an embedded correlative trial aim.
Methods:
DFCI 16-001 (NCT03020030) enrolled children ages 1-<22 years withde novo B- or T-cell ALL at 8 US and Canadian centers from 2017-2021. Participants <18 years were eligible to opt-in to the correlative HMH study at time of initial trial consent. Parents/guardians of participants completed surveys within 32-days of trial enrollment and longitudinally at 6-, 12-, and 24-months. Financial toxicity was the primary endpoint of interest for this secondary analysis, defined by two variables: (1) development of any new HMH domain (food, housing, or utility insecurity) at 6-24 months as compared to baseline and (2) catastrophic income loss defined as ≥25% annual household income loss at 6-24 months compared to baseline. Cumulative incidence of new HMH and catastrophic income loss in the presence of competing risks of coming off study (off-protocol therapy, death, relapse) were estimated using the Aalen-Johansen method. A subcohort analysis was conducted among participants who reported no HMH at baseline. Multivariable competing risk models evaluated the association of patient, household, and disease characteristics with risk of developing new HMH.
Results:
Among 422 participants (15% Hispanic and 7% non-Hispanic Black, 23% single-parent household, 40% annual household income <200% federal poverty level) with evaluable baseline survey data, 115 (27%) reported HMH at baseline. The cumulative incidence of any new HMH was 19.3% (95% CI: 15.9-23.5) at 6-months, 27.7% (95% CI: 23.8-32.4) at 12-months, and 30.0% (95% CI: 25.9-34.7) at 24-months. The cumulative incidence of catastrophic income loss was 20.3% (95% CI: 16.7-24.7) at 6-months, 28.6% (95% CI: 24.5-33.5) at 12-months, and 31.5% (95% CI: 27.2-36.5) at 24-months. Among the subcohort of 307 families with no baseline HMH, the cumulative incidences of any new HMH or catastrophic income loss at 24-months were 24.3% (95% CI: 19.9-29.6) and 27.9% (95% CI: 23.1-33.7), respectively. In multivariable modeling, children who identified as non-Hispanic Black (RR 3.5, 95% CI: 1.7-7.3), lived in a single-parent household (RR 2.1, 95% CI: 1.3-3.2), preferred a non-dominant language (i.e. non-English for US participants and non-English/French for Canadian participants, RR 2.1, 95% CI: 1.2-3.6), or had baseline household income <200% federal poverty level (RR 1.8, 95% CI: 1.1-2.9) were more likely to develop new HMH during treatment.
Conclusion:
Nearly a third of families of children receiving chemotherapy for ALL develop catastrophic financial toxicity during therapy including new unmet basic needs such as food insecurity, or ≥25% income loss. A majority experience this financial toxicity by 6-months into treatment, identifying a key inflection point for potential intervention. Importantly, nearly 1 in 4 families who had no HMH at the time of their child’s diagnosis developed HMH during therapy. These findings stress the clinical importance of longitudinal financial screening over the course of cancer treatment, given the high prevalence of new material needs that arise and the potential to address these needs with family-centered interventions. Future work will assess the impact of early financial toxicity on clinical outcomes in this population and focus on the development of interventions to mitigate the profound financial toxicity impacting families during leukemia care.
Keywords:
Clinical Trials, Lymphoid Malignancies, Supportive Care, Human, Study Population, Health Disparities Research, Lymphoid Leukemias, Health Economics, Patient-Reported Outcomes, Diseases, Clinical Research, ALL, Research, Treatment Considerations, Pediatric, Clinical Practice (Health Services And Quality)
https://www.audiomedica.com/wp-content/2025/12/251209-0900-Peihua-Lu-Robert-Chiesa-C2998-Discussion-at-ASH-AJO-PRODUCTION-MASTER.mp3Dramatic Remissions with “Off-the-Shelf” and “Base Edited” CAR T-cell Therapies in Children with Relapsed/Refractory T-Cell Malignancies
A discussion interview with Peihua Lu MD from Lu Daopei Hospital in Beijing, China and Robert Chiesa MD PhD from Great Ormond Street Hospital for Children, London, UK, at the American Society of Hematology Annual Meeting in Orlando, Florida, USA
ORLANDO, USA—Children and young adults whose T-cell malignancies had become refractory to all standard treatments have been rescued by means of two different chimeric antigen receptor T-cell therapies: one developed commercially in China and the other created in the laboratory of a leading children’s hospital in London by means of a new method of engineering DNA called: “base editing”.
At the 2025 American Society of Hematology annual meeting in Orlando, Florida, lead author of the Chinese study, Peihua Lu MD from Lu Daopei Hospital in Beijing and team-leader Robert Chiesa MD PhD from Great Ormond Street Hospital for Children, London, UK, met up with Audio Journal of Oncology anchor, Peter Goodwin, to discuss their pioneering early studies which seem to offer hope for patients and their families.
Audio Journal of Oncology: Peihua Lu MD and Robert Chiesa MD PhD
IN: “[GOODWIN] Welcome to…. OUT: ……..from all of us, Good-bye ” 33:51
A discussion on ASH ABSTRACTS at the 2025 Annual Meeting:
Abstract 1042: “CTD402, allogeneic anti-CD7 CAR t-cell, in relapsed or refractory (R/R) t-cell acute lymphoblastic leukemia/lymphoblastic lymphoma (T-ALL/LBL) – report of clinical outcomes at the recommended phase 2 dose (RP2D)”
Abstract 1041: “Universal base-edited CAR7 T cells for T-cell acute lymphoblastic leukemia”
An interview with Jeanne Tie MD, Medical Oncologist, Peter MacCallum Cancer Centre and Personalised Oncology Division, Walter and Eliza Hall Institute of Medical Research, Melbourne, Australia.
BERLIN, Germany—Liquid biopsy as a means of monitoring disease control in patients with stage three colon cancer has been investigated in a study from Melbourne, Australia reported to the 2025 Annual Congress of the European Society for Medical Oncology, ESMO. The aim was to discover whether patients with ctDNA negative biopsy findings could safely avoid chemotherapy and be spared toxicities including neuropathy.
After reporting findings from the AGITG DYNAMIC-III trial, lead author Jeanne Tie MD, who is a Medical Oncologist at the Peter MacCallum Cancer Centre in Melbourne, Australia, discussed the results with the Audio Journal of Oncology’s reporter, Peter Goodwin:
AUDIO JOURNAL OF ONCOLOGY with:Jeanne Tie MD. IN: “[GOODWIN] I am at the European Society for ….. OUT: …..Audio Journal of Oncology, I’m Peter Goodwin. 10:20 sec
ESMO 2025 ABSTRACT LBA9 (Presidential Symposium):
“ctDNA-guided adjuvant chemotherapy de-escalation in stage III colon cancer: Primary analysis of the ctDNA-negative cohort from the randomized AGITG DYNAMIC-III trial (Intergroup study of AGITG and CCTG)”
Speaker:
Jeanne Tie (Melbourne, Australia, VIC)
Authors:
Jeanne Tie (Melbourne, Australia, VIC) Yuxuan Wang (Baltimore, United States of America) Jonathan M. Loree (Vancouver, Canada) Joshua Cohen (Baltimore, United States of America) David Espinoza (Camperdown, Australia) Rachel Wong (Box Hill, Australia) Timothy J. Price (Woodville, Australia) Niall Tebbutt (Heidelberg, Australia) Matthew Burge (Herston, Australia) James Lynam (Waratah, Australia) Belinda Lee (Melbourne, Australia) Samuel J. Harris (Bendigo, Australia) Lorraine Chantrill (Wollongong, Australia) Daniel A. Breadner (London, Canada) Christopher O’Callaghan (Kingston, Canada) Chetan Bettegowda (Baltimore, United States of America) Nicholas Papadopoulos (Baltimore, United States of America) Kenneth Kinzler (Baltimore, United States of America) Bert Vogelstein (Baltimore, United States of America) Peter Gibbs (Parkville, Australia)
Background
Adjuvant chemotherapy (ACT) benefit is uncertain for any individual patient (pt). Post-surgery circulating tumour DNA (ctDNA) testing could support risk-adjusted treatment selection. The DYNAMIC-III study explored ACT de-escalation or escalation, informed by post-surgery ctDNA results.
Methods
In this multicentre, randomised, phase II/III trial, pts with stage III colon cancer underwent tumour-informed ctDNA testing 5-6 weeks post-surgery and were randomised (1:1) to ctDNA-guided or standard management. Clinicians pre-specified standard ACT. In the ctDNA-guided arm, ctDNA-negative results prompted ACT de-escalation: from 6 to 3 months of fluoropyrimidine (FP) or observation, from 3 months of doublet to single-agent FP, or from 6 months of doublet to 3 months doublet or single-agent FP. The primary endpoint was 3-year recurrence-free survival (RFS). A sample size of 750 provided 80% power with a one-sided 97.5% CI to demonstrate non-inferiority (NI) with a NI margin of 7.5%.
Results
Of 968 evaluable pts, 702 (72.5%) were ctDNA-negative; 353 assigned to ctDNA-guided and 349 to standard management. Median follow-up was 45 months. 319 (90.4%) pts received ctDNA-guided per-protocol de-escalation. Treatment de-escalation reduced oxaliplatin-based chemotherapy use versus standard management (34.8% vs 88.6%, P < 0.001) and lowered grade 3+ adverse events of special interest (6.2% vs 10.6%, P = 0.037) and treatment-related hospitalisation (8.5% vs 13.2%, P = 0.048). However, non-inferiority of ctDNA-guided de-escalation was not confirmed (3-year RFS, 85.3% vs 88.1%; difference = -2.8%; 97.5% lower CI = -8.0%). Pre-planned subgroup analysis suggested de-escalation may be non-inferior in clinical low-risk (T1-3N1) tumours (3-year RFS, 91.0% vs. 93.2%; difference = -2.2%; 97.5% lower CI = -7.2%).
Conclusions
Stage III colon cancer pts with negative post-surgery ctDNA had low recurrence risk. ctDNA-guided de-escalation is feasible, substantially reduces oxaliplatin exposure and adverse events, with outcomes approaching standard management, especially for clinical low-risk tumours.
Clinical trial identification
ACTRN12617001566325 Date registered: 21 November 2017.
Legal entity responsible for the study
Australasian GastroIntestinal Trials Group (AGITG).
Funding
Marcus Foundation, NHMRC, Virginia and Ludwig Fund for Cancer Research, Lustgarten Foundation, Conrad R Hilton Foundation, Sol Goldman Charitable Trust, NIH, Eastern Health Research Foundation (Zouki Research Grant), Canadian Cancer Society, Canadian Institutes of Health Research (CIHR).
Chemo-Free Regimen with Neoadjuvant CDK 4/6 Inhibition plus Endocrine Therapy Benefits Patients with High-Risk ER+ HER2- Early Breast Cancer
An interview with: Paul H Cottu MD PhD, Medical Oncologist and Associate Professor, Institute Curie, Paris, France
BERLIN, Germany—Patients with high-risk, hormone receptor positive, HER2 negative early breast cancers, who would typically be candidates for chemotherapy, had good clinical responses, high biological responses and good rates of surgery in a clinical trial using a chemotherapy-free neoadjuvant regimen consisting of letrozole hormone therapy plus abemaciclib CDK 4/6 inhibition.
Medical Oncologist Paul Cottu MD PhD from the Institute Curie in Paris, France, reported findings from RIBOLARIS trial at the 2025 Annual Congress of the European Society for Medical Oncology held in Berlin. At his poster during the conference he talked about the study findings with Audio Journal of Oncology reporter Peter Goodwin:
AUDIO JOURNAL OF ONCOLOGY Paul H Cottu MD PhD
IN: “[GOODWIN] I am at the European ….. OUT: …I’m Peter Goodwin 7:56secs
ESMO ABTRACT 296O:
“Risk of recurrence (ROR) after neoadjuvant ribociclib plus ET in clinically high-risk ER+/HER2− BC: Preliminary analysis of the SOLTI-RIBOLARIS trial”
Speaker: Paul H. Cottu (Paris, France)
Authors:
Paul H. Cottu (Paris, France) Aleix Prat (Barcelona, Spain) Tomás Pascual (Barcelona, Spain) Huilin Hu (East Hanover, United States of America) Estelle Roux (Basel, Switzerland, NJ) Francisco Javier Salvador Bofill (Seville, Spain) Joana M. Ribeiro (Villejuif, France) Isabel Blancas López-Barajas (Granada, Spain) Thomas Bachelot (Lyon, France) Jerome Lemonnier (Paris, France) Juan M. Ferrero-Cafiero (Barcelona, Spain) Pablo Tolosa Ortega (Madrid, Spain, Valencia) Antonio Mulero-Sánchez (Barcelona, Spain) Thayane Antoniolli Crestani (Brussels, Belgium) Roisin M. Connolly (Cork, Ireland, MD) Cynthia X. Ma (St. Louis, United States of America) Antonio C. Wolff (Baltimore, United States of America, MD) Guillermo Villacampa (Barcelona, Spain) Thibault De La Motte Rouge (Rennes, France) Joaquín Gavilá-Gregori (Valencia, Spain)
Background
The CDK4/6 inhibitors (CDK46/i) are approved for early-stage HR+/HER2− breast cancer (BC). The randomized neoadjuvant NeoPAL and CORALLEEN trials provided proof of concept that CDK4/6i in combination with endocrine therapy (ET) have similar activity to multi-agent chemotherapy in pts with luminal B-PAM50 based- BC subtype. The PAM50-derived ROR score was identified as an endpoint of interest after neoadjuvant CDK4/6i-ET. The RIBOLARIS trial was designed to evaluate whether pts with ROR-low disease following neoadjuvant ribociclib (RIB) and ET can safely omit adjuvant chemotherapy.
Methods
RIBOLARIS is an open-label, single-arm, multicenter trial in pts with primary operable stage II, grade 2/3, Ki67 ≥20%, HR+/HER2− BC who are candidates for adjuvant chemotherapy. The study evaluates safety and long-term efficacy of a non-chemo regimen (RIB-ET) in pts with tumors showing a ROR-low score after 6 neoadjuvant cycles of RIB-ET (600 mg/day 3 weeks ON/1 week OFF + ET: letrozol 2.5 mg/day) followed by surgery (within 10 days). Pts with ROR-med/high tumors will receive chemotherapy-based treatment followed by RIB-ET. This preplanned Interim Analysis analyzed safety and efficacy after 686 surgeries. We expected at least 40% of the pts to achieve a ROR-low score after neoadjuvant RIB-ET.
Results
Among the enrolled pts, baseline characteristics included: median age 57 (38-84), postmenopausal status 62%, tumor stage IIA 60%, node-negative 60%, and histological grade 2 74%. At data cut-off, 686 out of 1100 surgeries (62.4%) were performed. Interestingly, we observed that 361 pts (52.6%) achieved a ROR-low score (Mean 11.3, 95% CI 10.5-12.2), while 325 pts (47.4%) had a med/high ROR score (Mean 36.9, 95% CI 34.2-39.5). The most common grade 3-4 severity TEAEs were neutropenia (grade 3: 46.3%; grade 4: 3.5%) and transaminases increased (grade 3: 10.4%; grade 4: 1.5%).
Conclusions
These preliminary results from the RIBOLARIS trial confirm and extend the findings from CORALLEEN and NeoPAL trials, demonstrating that a subset of pts with early-stage HR+/HER2− BC achieve ROR-low disease after neoadjuvant RIB-ET and may be candidate to spare chemotherapy. There was no new safety signal.
Clinical trial identification
NCT05296746.
An interview with Li Zhang MD, Medical Oncologist and Full Professor, Sun Yat-sen University Cancer Center, Guangzhou, China
BERLIN, Germany—A doubling of progression-free survival, and highly statistically significant benefit for overall survival, has been achieved in patients with epidermal growth factor- (EGFR-) mutated non-small cell lung cancers that had become refractory to EGFR tyrosine kinase inhibitor therapy in a study in which treatment with the antibody drug conjugate (ADC) sacituzumab tirumotecan was compared with standard platinum-based chemotherapy.
At the 2025 Annual Congress of the European Society for Medical Oncology (ESMO) Professor Li Zhang MD, a medical oncologist and full professor at Sun Yat-sen University Cancer Center in Guangzhou, China, reported findings from the randomized, multi-center phase III OptiTROP-Lung04 study at a late-breaking session. After his talk he discussed the findings with Audio Journal of Oncology reporter, Peter Goodwin:
AUDIO JOURNAL OF ONCLOGY: Li Zhang MD
IN: “[GOODWIN] I’m here at ……OUT: …..I’m Peter Goodwin 8:42 secs
ESMO ABSTRACT LBA5:
Sacituzumab tirumotecan (sac-TMT) vs platinum-based chemotherapy in EGFR-mutated (EGFRm) non-small cell lung cancer (NSCLC) following progression on EGFR-TKIs: results from the randomized, multi-center phase III OptiTROP-Lung04 study
Speaker:
Li Zhang (Guangzhou, China)
Authors:
Li Zhang (Guangzhou, China) Wen Feng Fang (Guangzhou, China) Lin Wu (Changsha, China) Xiangjiao Meng (Jinan, China) Yu Yao (Xi’an, Shaanxi Province, China) Wei Zuo (Nanchang, China) Wenxiu Yao (Chengdu, China) Yanyan Xie (Nanning, China) Yu Zhang (Mianyang, China) Jiuwei Cui (Changchun, China) Yongchang Zhang (Changsha, China) Xingya Li (Zhengzhou, China) Wu Zhuang (Fuzhou, China) Jian Fang (Beijing, China) Qiming Wang (Zhengzhou, China) Wei Jiang (Nanning, China) Kai Li (Tianjin, China) Yina Diao (Chengdu, China) Junyou Ge (CHENGDU, China) Yunpeng Yang (Guangzhou, China)
Background
Sac-TMT is a TROP2 ADC developed with a novel linker to conjugate the payload, a belotecan-derivative topoisomerase I inhibitor. Sac-TMT demonstrated significant survival benefits over docetaxel in EGFRm NSCLC after failure of EGFR-TKI and platinum-based chemotherapy (Fang et al., BMJ 2025). Here, we first report the final PFS analysis and preplanned interim OS analysis results from the phase 3 OptiTROP-Lung04 study (NCT05870319).
Methods
Patients (pts) were randomized (1:1) to receive sac-TMT monotherapy (5 mg/kg Q2W) or chemotherapy (pemetrexed 500 mg/m2 + carboplatin AUC 5 or cisplatin 75 mg/m2 Q3W for 4 cycles followed by maintenance of pemetrexed). The primary endpoint was PFS assessed by blinded independent review committee (BIRC) with OS as a key secondary endpoint tested hierarchically.
Results
A total of 376 pts (median age 59.5 yrs; 39.6% male; 79.3% ECOG PS 1; 94.7% prior 3rd-generation EGFR TKI) were randomized to the sac-TMT (n=188) or chemotherapy (n=188) groups. At a median follow-up of 18.9 mo, 21.3% of pts (sac-TMT) vs 1.6% (chemotherapy) remained on treatment. Sac-TMT demonstrated highly statistically significant and clinically meaningful improvements in PFS and OS compared to chemotherapy (Table). Grade ≥ 3 TRAEs occurred in 49.5% and 52.2%, and TRSAEs in 7.4% and 17.0% of pts in sac-TMT and chemotherapy arms, respectively. No drug-related interstitial lung disease/pneumonitis occurred in either arm.
Sac-TMT (n=188) Chemotherapy (n=188)
Median PFS (BIRC), mo (95% CI) 8.3 (6.7 – 9.9) 4.3 (4.2 – 5.5)
HR (95% CI) 0.49 (0.39 – 0.62)
P-value <0.0001
12-mo PFS rate, %, (95% CI) 32.3 (25.5 – 39.2) 7.9 (4.4 – 12.8)
Median OS, mo (95% CI) NR (21.5 – NE) 17.4 (15.7 – 20.4)
HR (95% CI) 0.60 (0.44 – 0.82)
P-value 0.0006
Adjusted median OS*, mo (95% CI) NR (21.5 – NE) 17.2 (15.4 – 18.9)
HR (95% CI) 0.56 (0.41 – 0.77)
P-value 0.0002
ORR (BIRC), % (95% CI) 60.6 (53.3, 67.7) 43.1 (35.9, 50.5)
Median DOR (BIRC), mo (95% CI) 8.3 (6.2 – 10.0) 4.2 (3.0 – 4.4)
Data cutoff: Jul 06, 2025. P-value was presented as one-sided. *censored at the date of initiation of subsequent anti-tumor ADC drug therapy.
Conclusions
Sac-TMT is the first TROP2 ADC to significantly improve PFS and OS over platinum-based chemotherapy, with manageable safety in EGFR-TKI resistant NSCLC, positioning it as a potential new standard of care for this population.
Clinical trial identification
NCT05870319.
Legal entity responsible for the study
Sichuan Kelun-Biotech Biopharmaceutical Co., Ltd.
An interview with:
https://www.audiomedica.com/wp-content/2025/11/251019-Erwei-Song-ESMO-2025-PRODUCTION-MASTER.mp3, Director of Health Science Center, President, Sun Yat-sen Memorial Hospital, Guangzhou (SYSU), Guangzhou, China.
BERLIN, Germany—The open-label HORIZON-Breast01 phase-three study has reported early data showing that, for previously treated patients with advanced or metastatic breast cancer, progression-free survival improved from a median of 8.3 months with pyrotinib plus capecitabine standard of care to 30.6 months among patients in the experimental arm who received monotherapy with the new antibody drug conjugate (ADC) trastuzumab resetecan. Furthermore, the ADC had a favorable safety profile with low occurrence of interstitial lung disease (ILD).
Findings were reported at the 2025 Annual Congress of the European Society for Medical Oncology by Erwei Song MD PhD, Director of the Health Science Center, President, Sun Yat-sen Memorial Hospital, Guangzhou (SYSU), in Guangzhou, China. After his talk at the conference, Professor Song discussed the findings with Audio Journal of Oncology reporter Peter Goodwin:
Audio Journal of Oncology: Erwei Song MD PhD
IN: “[GOODWIN] I am at …… OUT: …….of Oncology, I’m Peter Goodwin. 7:42secs
ESMO ABSTRACT LBA19:
“SHR-A1811 versus pyrotinib plus capecitabine in human epidermal growth factor receptor 2-positive (HER2+) advanced/metastatic breast cancer (BC): A multicenter, open-label, randomized, phase III study (HORIZON-Breast01)”
Speaker: Erwei Song (Guangzhou, China)
Authors:
Erwei Song (Guangzhou, China) Herui Yao (Guangzhou, China) Huiping Li (Beijing, China) Yongmei Yin (Nanjing, China) Qing Yuan Zhang (Harbin, China) Shusen Wang (Guangzhou, China) Quchang Ouyang (Changsha, China) Tao Sun (Shenyang, Liaoning, China) Xiaojia Wang (Hangzhou, China) Weimin Xie (Nanning, China) Biyun Wang (Shanghai, China) Wei Li (Changchun, China) Min Yan (Zhengzhou, China) Cuizhi Geng (Shijiazhuang, China) Yuan Peng (Beijing, China) Yaping Yang (Guangzhou, China) Fangli Dong (Shanghai, China) Ying Zhang (Shanghai, China) Lin Cheng (Shanghai, China) Xiaoyu Zhu (Shanghai, China)
Background
SHR-A1811, a HER2-targeted antibody-drug conjugate, proved substantial single agent antitumor activity in heavily pretreated solid tumors as shown in a global phase 1 trial (J Clin Oncol. 2024). Here, we first report the interim analysis of SHR-A1811 versus pyrotinib plus capecitabine in HER2+ advanced/metastatic BC from the pivotal phase 3 HORIZON-Breast01 study.
Methods
Taxane- and trastuzumab-pretreated patients (pts) with HER2+ advanced/metastatic BC were randomized (1:1) to receive intravenous SHR-A1811 or oral pyrotinib plus capecitabine. The primary endpoint was PFS by blinded independent central review (BICR).
Results
As of Jun 30, 2025, 287 pts were randomized (SHR-A1811, n=142; pyrotinib plus capecitabine, n=145; IHC 3+: 76.1% vs. 71.7%; HR+: 47.9% vs. 47.6%; median lines of prior systemic treatments: 1 vs.1; prior pertuzumab: 71.8% vs. 72.4%), with median follow-up of 15.9 months (95% CI 14.6–17.1) for SHR-A1811, and 15.3 months (95% CI 14.3–16.6) for pyrotinib plus capecitabine. The PFS by BICR was significantly improved in the SHR-A1811 group than in the pyrotinib plus capecitabine group (30.6 months vs. 8.3 months; HR 0.22 [95% CI 0.15–0.34]; p<0.0001; table). Although the median OS was not yet reached, SHR-A1811 showed a clear OS benefit trend. Median treatment duration was 19.5 months (95% CI 17.3–NR) with SHR-A1811, 7.1 months (95% CI 5.6–9.2) with pyrotinib, and 7.5 months (95% CI 5.7–9.6) with capecitabine. Similar rates of TRAEs were observed. Interstitial lung disease (ILD) occurred only in 4 pts (2.8%) receiving SHR-A1811 (grade 1/2: 3 [2.1%]; grade 3: 1 [0.7%]).
Conclusions
SHR-A1811 exhibited significant PFS benefit and strong trend in OS benefit versus pyrotinib plus capecitabine in the second-line therapy in HER2+ advanced/metastatic BC, with favorable safety profile of low ILD occurrence.
Clinical trial identification
NCT05424835.
Legal entity responsible for the study
Jiangsu Hengrui Pharmaceuticals Co., Ltd.
Funding
Jiangsu Hengrui Pharmaceuticals Co., Ltd.
Disclosure
Dong, Y. Zhang, L. Cheng, X. Zhu: Financial Interests, Personal, Full or part-time Employment: Jiangsu Hengrui Pharmaceuticals Co., Ltd.
An interview with: Andrew Clamp MD, PhD, Consultant Medical Oncologist, Christie Hospital, Manchester, UK
BERLIN, Germany—An important therapeutic gain in terms of overall- and progression-free survival has been achieved merely by changing the chemotherapy dose schedule given to patients with high-risk stage three or four epithelial ovarian cancer.
This was reported from the ICON8B: GCIG phase-three randomised trial by Andrew Clamp MD PhD of the Christie Hospital in Manchester, England, at the 2025 Annual Congress of the European Society for Medical Oncology. Dr. Clamp discussed the findings with our reporter, Peter Goodwin.
Audio Journal of Oncology interview: Andrew Clamp MD, PhD
IN: “[GOODWIN] I’m at the European ….. OUT: ….Journal of Oncology, I’m Peter Goodwin” 7:21secs
https://www.annalsofoncology.org/article/S0923-7534(25)02624-9/pdf
ESMO ABSTRACT:
1064O – ICON8B: GCIG phase III randomised trial comparing first-line weekly dose-dense chemotherapy + bevacizumab to three-weekly chemotherapy + bevacizumab in high-risk stage III-IV epithelial ovarian cancer (EOC): Final overall survival (OS) analysis
Speaker: Andrew R. Clamp (Manchester, United Kingdom)
Authors: Andrew R. Clamp (Manchester, United Kingdom) Iain McNeish (London, United Kingdom) Domenico Radice (London, United Kingdom) Rosemary Lord (Liverpool, United Kingdom) Agnieszka Michael (Guildford, United Kingdom, Surrey) Audrey Cook (Cheltenham, United Kingdom) Roshan Agarwal (Northampton, United Kingdom, Northamptonshire) Axel Walther (Bristol, United Kingdom) Sarah P. Blagden (Oxford, United Kingdom) Dearbhaile O’Donnell (Dublin, Ireland) James D. Brenton (Cambridge, United Kingdom) Sudha Sundar (Birmingham, United Kingdom) Cristiana Sessa (Bellinzona, Switzerland) Laura R. Murphy (London, United Kingdom) Francesca Schiavone (London, United Kingdom) Aleksandra Gentry-Maharaj (London, United Kingdom) Richard S. Kaplan (London, United Kingdom) Mahesh K. Parmar (London, United Kingdom, London) Jonathan A. Ledermann (London, United Kingdom)
ESMO Abstract
Background
In ICON8B the use of dose-dense weekly paclitaxel (ddwT) with 3-weekly (q3w) carboplatin (C) and bevacizumab (BEV) as first-line treatment improved median progression-free survival (PFS) by 5.5 months (m) compared to standard q3w paclitaxel (T) dosing with C+BEV (22.2m vs 16.7m; Hazard Ratio (HR) 0.75, 95% CI 0.62-0.90 p=0.002). We now report the final OS analysis conducted at trial closure.
Methods
Eligible participants (pts) with high-risk stage III (residual disease >1cm diameter after immediate primary surgery (IPS) or requirement for primary chemotherapy) or stage IV EOC were randomised 1:1:1 to Arm B1 (standard- q3w C AUC5/6+q3w T 175mg/m2+ q3w BEV 7.5mg/kg); Arm B2- (q3w C AUC5/6+ddwT 80mg/m2); Arm B3- (q3w C AUC5/6+ddwT 80mg/m2+ q3w BEV 7.5mg/kg). Up to six cycles chemotherapy and 18 BEV cycles were administered. Arm B2 recruitment discontinued after ICON8 saw no evidence of PFS improvement with q3wCddwT vs q3wCT. OS was a key secondary outcome and pts were followed for survival endpoints until trial closure on 18th Dec 2024 at end of academic funding.
Results
From 07/2015 to 03/2020 579 pts were randomised to arms B1 + B3. Median age was 64 years; 91% had High Grade Serous Carcinoma; 93% Stage IIIc/IV; 84% primary chemotherapy with planned delayed primary surgery, 14% IPS, 2% inoperable; 50.2% cases sequenced for germline BRCA1/2 mutations. After a median follow-up of 72.0m, 411 deaths were reported (197 in B3; 214 in B1). Median OS was 49.8m (95% CI 43·7-54.5m) in B3 and 39.6m (95% CI 34·7-45·0m) in B1 (HR 0·79, 95% CI 0·65-0·95, p=0·010). In pts receiving primary chemotherapy, median OS was 47.3m (95% CI 42.0-52.6m) in B3 and 37.1m (95% CI 32.3-42.1m) in B1.
Conclusions
In pts with high-risk stage III-IV EOC, the use of ddwT in combination with q3w C + BEV as first-line systemic therapy improves median OS by 10.2m compared to q3w T dosing. ddwT with q3wC+BEV should now be considered a standard-of-care first-line treatment option in this group. Further research is required to determine whether efficacy of this regimen is impacted by tumour homologous recombination deficiency and intrinsic chemosensitivity.
Clinical trial identification
ISRCTN10356387.
Legal entity responsible for the study
University College London.
Funding
Cancer Research UK and Medical Research Council.
An interview with Nima Nabavizadeh MD, Associate Professor of Radiation Medicine, Oregon Health & Science University (OHSU), Portland, USA, Chief Medical Officer, Cancer Early Detection Research Center, Portland, Oregon.
https://www.audiomedica.com/wp-content/2025/11/251107-Nima-Nabavizadeh-MD-ESMO-2024-PRODUCTION-MASTER.mp3
BERLIN, Germany—A pan-cancer early detection test, that identifies “methylation fingerprints” for a wide range of cancers, has been shown to find more cancers sooner than conventional screening according to research reported to the European Society for Medical Oncology (ESMO) 2025 Annual Congress.
Nima Nabavizadeh MD, Associate Professor of Radiation Medicine at the Oregon Health & Science University (OHSU) in Portland, USA, who is also Chief Medical Officer of the Cancer Early Detection Research Center in Portland, Oregon gave a report on the safety and performance of the test at the ESMO congress. Afterwards he spoke with our reporter, Peter Goodwin:
Audio Journal of Oncology: Nima Nabavizadeh MD
IN: “[GOODWIN]I am at the ESMO meeting …. OUT: ……of oncology. I’m Peter Goodwin” 9:55sec
ESMO ABSTRACT LBA64:
Safety and performance of a multi-cancer early detection (MCED) test in an intended-use population: Initial results from the registrational PATHFINDER II study
https://assets.grail.com/wp-content/uploads/2025/10/ESMO-2025_PF2-Initial-Results_Presentation_FINAL-CLEAN-10.16.2025.pdf
Speaker:
Nima Nabavizadeh (Portland, United States of America)
Authors:
Nima Nabavizadeh (Portland, United States of America) Charles McDonnell III (Sacramento, United States of America) Dax Kurbegov (Nashville, United States of America) Marc Matrana (New Orleans, United States of America) Shirish Gadgeel (Detroit, United States of America) Raymond H. Kim (Toronto, Canada) Gretchen Stipec (Fountain Valley, United States of America) Kevin Oeffinger (Durham, United States of America) Michael J. Demeure (Newport Beach, United States of America) Roland Matthews (Atlanta, United States of America) Rebecca Kaltman (Fairfax, United States of America) Tamar Toronjadze (Flushing, United States of America) Cora N. Sternberg (New York, United States of America) Jennifer Tran (Washington, United States of America) Natalia Colocci (Mountain View, United States of America) Leonardo Forero (Amarillo, United States of America) Margarita Lopatin (Menlo Park, United States of America) Margaret McCusker (Menlo Park, United States of America) Karthik Giridhar (Rochester, United States of America)
Background
The MCED test (Galleri®) detects cancer signals from cell-free DNA in blood and predicts cancer signal origin (CSO) to guide diagnostic (dx) evaluation. PATHFINDER 2 (PF2; NCT05155605) assesses its safety and performance in a large, diverse intended-use population.
Methods
PF2 is a prospective, multicenter, interventional study that enrolled participants (ppts) aged ≥50y with no clinical suspicion of cancer and no cancer diagnosis/treatment in the past 3y. Primary objectives were safety and performance of the MCED test. Ppts with an MCED cancer signal detected (positive) result underwent dx evaluation based on predicted CSO(s). This prespecified initial analysis included ppts with 12m follow-up (fu) as of Dec 31, 2024. A 3y fu is planned.
Results
35,878 ppts were enrolled. Of 23,161 performance analyzable ppts with 12m fu, 216 (0.93%) had a positive MCED test. Specificity was 99.6% (95% CI 99.5-99.7%); positive predictive value (PPV) was 61.6% (54.9-67.8%). First CSO prediction accuracy was 91.7% (85.8-95.3%). Episode sensitivity during 12m fu was 73.7% (65.6-80.4%) in a prespecified subgroup of 12 cancers responsible for ⅔ of US cancer deaths and 40.4% (35.3-45.8%) in all cancers. Of 329 ppts with cancer, 200 had screen-detected cancers: 133 by MCED testing (114 new primaries; 19 recurrent), 20 by USPSTF A/B and 47 by USPSTF C recommended screening tests. Of 133 MCED-detected cancers (MCED cancer detection rate: 0.57%), 75.2% do not have common screening options. Of 114 MCED-detected new primaries, 53.5% were stage I-II; 69.3% were stage I-III. Median time to dx resolution was 46d (IQR 42-59). Of 25,114 safety analyzable ppts, 159 (0.6%) had a protocol-directed invasive procedure. Invasive procedures were ∼2x more common for ppts dx with cancer vs not dx after a positive MCED test.
Conclusions
MCED testing increased the number of screen-detected cancers nearly 7-fold when added to USPSTF A/B recommended screening (3-fold when added to USPSTF A/B/C). Most MCED-detected new primaries were early stage. With PPV exceeding that of standard of care screening tests and a favorable safety profile, these initial PF2 results support the MCED test’s use for population-scale screening.
Clinical trial identification
NCT05155605.
Editorial acknowledgement
Medical writing support for the development of this abstract, under the direction of the authors, was provided by Jennifer Hepker, PhD, and Alexandra L. Thomas, PhD, of Citrus Health Group (Chicago, IL, USA), and was funded by GRAIL, Inc.
An interview with: Xiuning Le MD PhD, Medical Oncologist, Department of Thoracic Medicine, UT MD Anderson Cancer Center, Houston TX
BERLIN, Germany—Mutations in the HER2 molecule can be found in a few per cent of non-small cell lung cancers, and these can now be targeted by the new drug sevabertinib that can bring benefit to patients who have the mutation. That’s according to findings from the SOHO-01 study reported at the 2025 Annual Congress of the European Society of Clinical Oncology.
After her talk at the congress, first author Xiuning Le MD PhD, who is a medical oncologist in the Department of Thoracic Medicine, at the University of Texas MD Anderson Cancer Center, in Houston, talked about the new data with Audio Journal of Oncology reporter Peter Goodwin:
Audio Journal of Oncology; Xiuning Le MD PhD
IN: “[GOODWIN] I am at the European Society for Medical ….OUT: ……. For the Audio Journal of Oncology, I’m Peter Goodwin” 10: 18secs
2025 ESMO Berlin ABSTRACT LBA75:
Sevabertinib (BAY 2927088) in advanced HER2-mutant non-small cell lung cancer (NSCLC): Results from the SOHO-01 study
Speaker: Xiuning Le (Houston, United States of America)
Authors: Xiuning Le (Houston, United States of America) Tae Min Kim (Seoul, Republic of Korea) Xiaorong Dong (Wuhan, China) Herbert Ho Fung Loong (Hong Kong, Hong Kong SAR, China) Nicolas Girard (Paris, France) Shun Lu (Shanghai, China) Hye Ryun Kim (Seoul, Republic of Korea) Boon-Cher Goh (Singapore, Singapore) Arsela Prelaj (Milan, Italy) Yong Fang (Hangzhou, China) Lin Wu (Changsha, China) Yuki Shinno (Tokyo, Japan) Gennaro Daniele (Rome, Italy) Tsung-Ying Yang (Taichung City, Taiwan) Gerrina Ruiter (Amsterdam, Netherlands) Jun Zhao (Beijing, China) Jan Christoph Brase (Basel, Switzerland) Rui Li (Whippany, United States of America) Paolo Grassi (Milan, Italy) Lin Li (Beijing, China)
Background
Sevabertinib is a potent, reversible, oral HER2 tyrosine kinase inhibitor with FDA Breakthrough Therapy Designation and Priority Review for pretreated patients (pts) with advanced HER2-mutant NSCLC. We report updated efficacy and safety in pretreated and treatment-naïve pts with HER2-mutant NSCLC in the open-label, multicenter Phase I/II SOHO-01 study.
Methods
Pts with HER2-mutant NSCLC were treated with sevabertinib 20 mg twice daily in 3 cohorts: Cohort D, previous systemic therapy but naïve to HER2 ex20ins-targeted therapy; Cohort E, previous HER2-targeted antibody-drug conjugates; Cohort F, naïve to systemic anti-cancer therapy for advanced disease. The primary endpoint was objective response rate (ORR) by RECIST v1.1 and blinded independent central review. Secondary endpoints were duration of response (DoR) and progression-free survival (PFS).
Results
At the data cut-off (June 27, 2025), 209 pts with HER2-mutant NSCLC were treated: 81 (D), 55 (E), and 73 (F). ORR (95% CI) was 64% (53, 75; D), 38% (25, 52; E), and 71% (59, 81; F). Median (95% CI) DoR was 9.2 (6.3, 13.5; D), 8.5 (5.6, 16.4; E), and 11.0 (8.1, not evaluable; F) months; 12-month DoR rates (95% CI) were 42% (27, 57; D) and 29% (5, 53; E). Median PFS (95% CI) was 8.3 (6.9, 12.3; D) and 5.5 (4.3, 8.3; E) months, and not reached (F). In Cohort D, pts with baseline brain metastases had a similar ORR to those without (61% vs 65%). Among pts with HER2 tyrosine kinase domain (TKD) mutations, those with Y772_A775dupYVMA had a higher ORR (78% vs 57%) and median PFS (12.2 vs 7.0 months) than those with other HER2 TKD mutations. Overall, grade ≥3 treatment-related adverse events (TRAEs) were reported in 31% of pts. Diarrhea was the most commonly reported TRAE, mostly grade 1/2 (grade 3: 14%). TRAEs led to treatment discontinuation in 3% of pts; none due to diarrhea. There were no reports of interstitial lung disease or pneumonitis.
Conclusions
Sevabertinib showed rapid and durable responses with a manageable safety profile in pretreated and treatment-naïve pts with advanced HER2-mutant NSCLC. These data support sevabertinib as a potential practice-changing, new targeted therapy for pts with HER2-mutant NSCLC.
Clinical trial identification: NCT05099172, March 28, 2025.
Editorial acknowledgement: Alice Xue, MSc, Erica Sedgwick, MSc, and Rachel Fairbanks, BA, of Caudex, IPG Health Medical Communications, provided medical writing and editorial assistance in the development of this abstract, funded by Bayer AG.
Legal entity responsible for the study: Bayer AG.
New England Journal of Medicine
https://www.nejm.org/doi/full/10.1056/NEJMoa2511065
An interview with: Christof Vulsteke MD PhD, Medical Oncologist, Head of the Integrated Cancer Center Ghent, Belgium
BERLIN, Germany—Patients with muscle invasive bladder who were ineligible for cisplatin chemotherapy gained large, clinically meaningful and statistically significant benefits from treatment with the antibody drug conjugate enfortumab vedotin combined with pembrolizumab checkpoint inhibition in the phase three KEYNOTE-905 study.
At the 2025 Annual Congress of the European Society for Medical Oncology (ESMO) Medical Oncologist Christof Vulsteke, Head of the Integrated Cancer Centre in Ghent, Belgium, reported marked improvements of event-free and overall survival among patients treated with the new combination, in comparison with those receiving standard radical cystectomy plus pelvic lymph node dissection. After his talk in Berlin he gave more details to Audio Journal of Oncology reporter Peter Goodwin:
Audio Journal of Oncology: Christof Vulsteke MD PhD; IN: “[GOODWIN] I am at the ESMO meeting in Berlin ……OUT: …Goodwin for the Audio Journal of Oncology, Goodbye 7:12 secs
ESMO 2025 ABSTRACT No. LBA2
“Perioperative (periop) enfortumab vedotin (EV) plus pembrolizumab (pembro) in participants (pts) with muscle-invasive bladder cancer (MIBC) who are cisplatin-ineligible: The phase III KEYNOTE-905 study”
Speaker: Christof Vulsteke (Gent, Belgium)
Authors:
Christof Vulsteke (Gent, Belgium) Hristos Kaimakliotis (Indianapolis, United States of America) Pongwut Danchaivijitr (Bangkok, Thailand) Maksym Y. Sabadash (Lviv, Ukraine) Alejo Rodriguez-Vida (Barcelona, Spain) Zhentao Zhang (Fort Wayne, United States of America) Vagiz Atduev (Nizhny Novgorod, Russian Federation) Yunus Emre Goger (Konya, Türkiye) Steffen Rausch (Tuebingen, Germany) Seok Ho Kang (Seoul, Republic of Korea) Yohann Loriot (Villejuif, France) Jens Bedke (Stuttgart, Germany) Matthew D. Galsky (New York, United States of America) Peter H. O’Donnell (Chicago, United States of America) Michael Mihm (Chicago, United States of America) Changting Meng (Groton, United States of America) David Huang (Rahway, United States of America) Chethan Ramamurthy (North Wales, United States of America) Blanca Homet Moreno (Madrid, Spain) Anders Ullén (Stockholm, Sweden)
Background
Radical cystectomy + pelvic lymph node dissection (RC + PLND) is the standard treatment for pts with MIBC who are cisplatin-ineligible. Periop therapy may improve outcomes in these pts.
Methods
The phase 3 KEYNOTE-905/EV-303 study (NCT03924895) evaluated efficacy and safety of periop EV + pembro and RC + PLND vs RC + PLND in adult pts with MIBC (T2-T4aN0M0 or T1-T4aN1M0) who were cisplatin-ineligible or declined cisplatin. Pts were randomized 1:1 to EV + pembro (3 cycles EV 1.25 mg/kg on d1 and d8 + pembro 200 mg on d1 Q3W, followed by RC + PLND, then 6 cycles EV + 14 cycles pembro) vs control (RC + PLND only). Study therapy continued until progression, unacceptable adverse events (AEs), withdrawal of consent, or completion of planned treatment. The primary endpoint was event-free survival (EFS) by blinded independent central review. Secondary endpoints were overall survival (OS; key), pathological complete response (pCR) rate (key), and safety.
Results
170 pts were randomized to EV + pembro and 174 pts to control. >80% of pts were cisplatin-ineligible per Galsky criteria. As of Jun 6, 2025, median follow-up time was 25.6 mo (range, 11.8–53.7). 149 pts (87.6%) in the EV + pembro arm and 156 (89.7%) in the control underwent surgery. EV + pembro significantly improved EFS (median not reached [NR] vs 15.7 mo; HR 0.40; 95% CI 0.28–0.57; P<.001), OS (NR vs 41.7 mo; HR 0.50; 95% CI 0.33–0.74; P<.001), and pCR rate (57.1% vs 8.6%; estimated difference 48.3%; 95% CI 39.5–56.5; P<.001) vs control. Treatment-emergent AEs occurred in 100% (gr ≥3, 71.3%) of pts in the EV + pembro arm and 64.8% (gr ≥3, 45.9%) in the control. Most frequent gr ≥3 AE of special interest (based on distinct prespecified lists for each drug) was severe skin reactions (grouped term; 11.4%) for pembro, and skin reactions (grouped term; 10.8%) for EV.
Conclusions
Adding periop EV + pembro to surgery significantly and meaningfully improved EFS, OS, and pCR rate in pts with MIBC who were predominantly cisplatin-ineligible. The safety profile of EV + pembro was manageable and consistent with prior reports. This is the first perioperakthrough regimen to improve outcomes vs RC + PLND in this setting and may be a new standard of care.
Clinical trial identification: NCT03924895.
An interview with: Xichun Hu MD PhD, Professor, Director, Department of Medical Oncology, Shanghai Cancer Center, Fudan University, Shanghai, China
BERLIN, Germany—In a head-to-head comparison of two antibody drug conjugates used to treat unresectable or metastatic breast cancer, patients treated with trastuzumab botidotin lived more than twice as long before disease progression than those in the control arm receiving trastuzumab emtansine (T-DM1). This finding was announced by Chinese researchers at the 2025 Annual Congress of the European Society of Medical Oncology.
Lead author Xichun Hu MD PhD, Professor, Director, Department of Medical Oncology, Shanghai Cancer Center, Fudan University, Shanghai, China talked about the findings of his groups phase three randomized controlled study with Audio Journal of Oncology reporter Peter Goodwin:
AUDIO JOURNAL OF ONCOLOGY: Xichun Hu MD PhD
IN: “[GOODWIN] Peter Goodwin at ESMO ..OUT: ..of Oncology, I’m Peter Goodwin 8:30 sec
ESMO ABSTRACT LBA24
“Trastuzumab botidotin vs trastuzumab emtansine (T-DM1) in HER2-positive unresectable or metastatic breast cancer: Results from a randomized phase III study”
Speaker: Xichun Hu (Shanghai, China)
Authors:
Xichun Hu (Shanghai, China) Jian Zhang (Shanghai, China) Quchang Ouyang (Changsha, China) Qingyuan Zhang (Harbin, China) Huihui Li (Jinan, China) Xu Wang (Tianjin, China) Ying Wang (Guangzhou, China) Yongmei Yin (Nanjing, China) Shusen Wang (Guangzhou, China) Yuanting Gu (Zhengzhou, Algeria) Tao Sun (Shenyang, China) Jingfen Wang (Linyi, China) Xinhong Wu (Wuhan, China) Fanfan Li (Hefei, China) Xi Chen (Fuzhou, China) Man Li (Dalian, China) Jin Yang (Xi’an, Shaanxi Province, China) Hua Yang (Baoding, China) Xiaoping Jin (Chengdu, China) Junyou Ge (CHENGDU, China)
Lecture Time
ASTRACT
Background
Trastuzumab botidotin (A166) is a HER2-directed ADC developed using a stable, protease-cleavable valine-citrulline linker conjugated to the anti-microtubule agent Duo-5. In a phase 1 study, A166 showed promising activity in heavily pretreated patients (pts) with HER2+ breast cancer (BC). Here, we first report the results from a phase 3 study (NCT06968585).
Methods
Pts with HER2+ unresectable or metastatic BC who had received at least one prior anti-HER2 therapy were randomized (1:1) to receive A166 (4.8 mg/kg Q3W) or T-DM1 (3.6 mg/kg Q3W) until disease progression or unacceptable toxicity. The primary endpoint was PFS by BICR per RECIST v1.1.
Results
A total of 365 pts were randomized (median age 55 years; 73.4% with visceral metastases; 53.4% received ≥2 prior anti-HER2 therapies; 55.9% had prior pyrotinib). As of 26 April 2025, median follow-up was 14.9 mo. Median PFS was significantly longer in A166 than in T-DM1 (11.1 mo vs 4.4 mo; HR 0.39 [95% CI 0.30-0.51], p<0.0001). PFS benefit with A166 was consistently observed regardless of prior lines of anti-HER2 therapy (HR 0.36 for 1 prior line; HR 0.39 for ≥2 prior lines). ORR by BICR was 76.9% vs 53.0%, and mDOR was 12.2 mo vs 5.7 mo. Although OS data were immature, a trend toward benefit was observed in A166 (HR 0.62; 95% CI, 0.38-1.03). Grade ≥3 TEAEs occurred in 69.8% of pts in A166 and 63.7% in T-DM1. The most common grade ≥3 TEAEs (≥5%) were corneal disorder, dry eye, and vision blurred in A166, and platelet count decreased, neutrophil count decreased, hypokalemia, and GGT increased in T-DM1. Among A166-treated pts who experienced any-grade ocular AEs, instrumental activities of daily living (ADL) limitations occurred in 37 (20.3%) pts, and self-care ADL limitations in 13 (7.1%) pts; these resolved in 32 (86.5%) and 12 (92.3%) pts, respectively. TEAEs led to discontinuation in 1.1% of pts in A166 and 3.8% in T-DM1. No TEAE led to death in A166, compared with 1.1% in T-DM1.
Conclusions
A166 demonstrated statistically significant and clinically meaningful improvement in PFS compared with T-DM1, with a manageable safety profile in pts with HER2+ unresectable or metastatic BC. These results position A166 as a potential new therapeutic option for HER2+ disease.
Clinical trial identification
NCT06968585.
Legal entity responsible for the study
Sichuan Kelun-Biotech Biopharmaceutical Co., Ltd.
Funding
Sichuan Kelun-Biotech Biopharmaceutical Co., Ltd.
Disclosure
Jin, J. Ge: Financial Interests, Institutional, Full or part-time Employment: Sichuan Kelun-Biotech Biopharmaceutical Co., Ltd. All other authors have declared no conflicts of interest.
Xichun Hu MD, PhD
Medical Oncology
Xuhui, Shanghai, China
Xi-Chun Hu, M.D., Ph. D., is currently a Professor, Director of the Department of Medical Oncology, Shanghai Cancer Center, Fudan University, Shanghai, China. Dr. Hu has published more than 170 papers in the journals, such as Lancet Oncology, JCO, and International Journal Cancer, and 5 book chapters. He is vice editor of the ABC (Advanced breast cancer) guideline (Chinese version) and one of the leading authors of the CBCS (Chinese Breast Cancer Society) guideline for breast cancer diagnosis and treatment which is updated biannually.
Dr. Hu is an active member of the American Society of Clinical Oncology, General secretary & Member of the standing committee of CBCS (Chinese Breast Cancer Society), Vice-chair of Shanghai Breast Cancer Society, Member of the Standing Academic Committee of CSCO (Chinese Society of Clinical Oncology).
Dr. Hu’s major interest is in the diagnosis and management of breast cancer, both in the clinic and in the laboratory, and in phase I trial on new anticancer agents. His laboratory interests and contributions have been in the area of serum tumor markers, epigenetic alteration and gene expression, and detection of residual disease. He and his laboratory are now concentrating on translational research on triple-negative breast cancer and angiogenesis.
An interview with: Martin Wermke MD, TU Dresden, NCT/UCC Early Clinical Trial Unit and Medical Clinic, Poliklinik I, Natural Centre for Tumor Diseases, Dresden, Germany
BERLIN, Germany—The prospect of markedly better outcomes for patients with small cell lung cancer, with “encouraging initial survival outcomes”, was raised by findings from the DeLLphi-303 study, reported at the European Society for Medical Oncology (ESMO) 2025 Annual Congress. The bi-specific T-cell engager drug tarlatamab was included with initial therapy for patients with extensive stage small cell lung cancer.
Martin Wermke MD, from TU Dresden, Director of the NCT/UCC Early Clinical Trial Unit and of the Medical Clinic, Poliklinik I, Natural Centre for Tumor Diseases in Dresden, Germany reported the latest study data to the ESMO congress. After his talk he gave the details to our reporter Peter Goodwin:
Audio Journal of Oncology; Martin Wermke MD: ”[GOODWIN] Peter Goodwin here at the ESMO meeting ………….of Oncology, I’m Peter Goodwin.” 6:16secs
https://pubmed.ncbi.nlm.nih.gov/40934933/
ESMO ABSTRACT 2757O
Tarlatamab with first-line chemoimmunotherapy for extensive stage small cell lung cancer (ES-SCLC): DeLLphi-303 study
Speaker: Martin Wermke (Dresden, Germany)
Authors
Martin Wermke (Dresden, Germany) Sally Lau (Toronto, Canada) Mor T. Moskovitz (Petah Tikva, Israel) Ingel Demedts (Roeselare, Belgium) Kelly Paulson (Seattle, United States of America) Aurélie Swalduz (Lyon, France) Cornelius Waller (Freiburg, Germany) Luis Paz-Ares (Madrid, Spain) Makoto Nishio (Koto-ku, Japan) Michael Boyer (Camperdown, Australia, NSW) James Chih-Hsin Yang (Taipei City, Taiwan) Amanda Parkes (Thousand Oaks, United States of America) Yuyang Zhang (Thousand Oaks, United States of America) Ali Hamidi (Thousand Oaks, United States of America) Mukul Minocha (Thousand Oaks, United States of America) Pedro F. Simoes da Rocha (Barcelona, Spain)
Background: Tarlatamab with anti-PD-L1 achieved notable survival outcomes with manageable safety as maintenance therapy following 1L platinum-etoposide chemotherapy and anti-PD-L1 (1L chemo-IO) for ES-SCLC. In this phase Ib study (parts 2, 4, 7), the safety and efficacy of adding tarlatamab to 1L chemo-IO was assessed.
Methods: Patients (pts) had received 1 cycle of 1L chemo-IO prior to enrollment. On study, pts received 3 cycles of tarlatamab + 1L chemo-IO followed by tarlatamab + anti-PD-L1 Q3W until progression. Tarlatamab was administered 20 mg Q3W with a 1 mg step dose. Primary endpoints included dose-limiting toxicities (DLTs), treatment-emergent (TE), and treatment-related (TR) adverse events (AEs). Key secondary endpoints were objective response (OR), duration of response (DOR), progression-free survival (PFS), and overall survival (OS).
Results: Of 96 pts enrolled, 3 (3%) had DLTs. TEAEs and TRAEs were reported in all pts. The most common TRAEs were cytokine release syndrome (CRS, 56%), anemia (54%), and dysgeusia (46%). Grade (Gr) ≥ 3 TRAEs occurred in 72 pts (75%), most commonly neutropenia/neutrophil count decreased (44%), anemia (23%), and lymphopenia/lymphocyte count decreased (11%), primarily within the first two cycles. CRS (54% Gr 1-2; 2% Gr 3-4) and ICANS and associated neurological events (5% Gr 1-2; 1% Gr 3) TRAEs were mostly low grade. Other immune-related AEs were rare (2%). From a baseline scan after 1 cycle of 1L chemo-IO, OR rate following tarlatamab addition to 1L chemo-IO was 71%, with median DOR of 11.0 months (mo) (95% CI 6.7-not estimable). Median PFS was 9.0 mo. With a median follow-up time of 11.3 mo, the Kaplan-Meier estimate of OS at 12 mo was 81% (Table). Results from further follow-up will be presented. Table: 2757O
Safety and efficacy of tarlatamab + chemoimmunotherapy as 1L treatment for ES-SCLC
Conclusions: The combination of tarlatamab with chemo-IO for 1L treatment of ES-SCLC demonstrated manageable safety with encouraging initial survival outcomes, supporting further investigation of this combination in the phase III DeLLphi-312 study.
Clinical trial identification: NCT05361395.
Editorial acknowledgement
Medical writing support for the development of this abstract was provided by Sukanya Raghuraman, PhD, of Cactus Life Sciences, part of Cactus Communications, and Liz Leight, PhD, an employee of Amgen Inc., and was funded by Amgen Inc.
Legal entity responsible for the study: Amgen Inc.
Funding: Amgen Inc.
An interview with: John P. Crown MD MBA, Consultant Medical Oncologist, St. Vincent’s University Hospital, Dublin, Professor of Translational Cancer Research, Dublin City University, Professor of Medicine, University College Dublin Ireland.
BERLIN, Germany—Patients with high-risk node-negative ER-positive HER2-negative early breast cancer who had the CDK 4/6 inhibitor drug ribociclib added to their non-steroidal aromatase inhibitor (AI) adjuvant therapy after surgery had significantly longer freedom from progression to invasive disease compared with patients receiving the AI alone. This is according to five-year data from the NATALEE trial reported at the 2025 Annual Congress of the European Society for Medical Oncology.
Professor John P. Crown MD MBA, Consultant Medical Oncologist, from St. Vincent’s University Hospital in Dublin gave reporter Peter Goodwin the latest details:
Audio Journal of Oncology, John P. Crown MD MBA,
IN: “[GOODWIN] I am at the ESMO meeting, 2025, in Berlin ….OUT: signing off for the Audio Journal of Oncology.” 11:24 secs
2025 ESMO: Proffered Paper Friday 14:00 Oct 17, 2025
Abstract Title:
LBA14 – Adjuvant ribociclib (RIB) plus nonsteroidal aromatase inhibitor (NSAI) in patients (pts) with HR+/HER2− early breast cancer (EBC): NATALEE 5-year outcomes
Speaker:
John P. Crown (Dublin, Ireland)
Authors:
John P. Crown (Dublin, Ireland) Daniil Stroyakovskiy (Moscow, Russian Federation) Denise Yardley (Chattanooga, United States of America) Chiun-Sheng Huang (Taipei City, Taiwan) Peter A. Fasching (Erlangen, Germany) Aditya Bardia (Los Angeles, United States of America) Stephen Chia (Vancouver, Canada) Seock-Ah Im (Seoul, Republic of Korea) Miguel Martin (Madrid, Spain) Binghe Xu (Beijing, China) Carlos H. Barrios (Porto Alegre, Brazil) Michael Untch (Berlin, Germany) Rebecca Moroose (Lake Mary, United States of America) Sara A. Hurvitz (Seattle, United States of America, CA) Gabriel N. Hortobagyi (Houston, United States of America) Dennis Slamon (Los Angeles, United States of America) Frances Visco (Washington, United States of America) Gonzalo Spera (Montevideo, Uruguay) Zheng Li (East Hanover, United States of America) Sherene Loi (Melbourne, Australia, VIC)
Background:
The phase 3 NATALEE trial demonstrated that adjuvant RIB + NSAI led to a statistically significant invasive disease–free survival (iDFS) benefit in pts with stage II and III HR+/HER2− EBC. We present a protocol-specified 5-year efficacy analysis.
Methods:
Pts with HR+/HER2− EBC were randomized 1:1 to RIB (400 mg/d; 3 weeks on/1 week off for 3 y) + NSAI (letrozole 2.5 mg/d or anastrozole 1 mg/d for 5 y) or NSAI alone. Men and premenopausal women received goserelin. Pts were included if they had anatomical stage IIA (if N1 [1-3 axillary lymph nodes] or N0 with additional high-risk factors), stage IIB, or stage III disease per AJCC, 8th ed. The primary end point of iDFS and secondary efficacy end points of distant disease–free survival (DDFS), distant relapse–free survival (DRFS), and overall survival (OS) were evaluated using Kaplan-Meier methods. Statistical comparisons were made by stratified log-rank test.
Results:
At data cutoff (May 28, 2025), all pts were off RIB treatment, and a similar proportion had completed 5 years of NSAI treatment in both arms (RIB + NSAI, 36.5%; NSAI alone, 34.4%). With a median iDFS follow-up of 55.4 months, RIB + NSAI demonstrated persistent iDFS benefit over NSAI alone (hazard ratio [HR], 0.716; 95% CI: 0.618-0.829; nominal 1-sided P<.0001). Absolute iDFS rates were 90.8% vs 88.0% at 3 y, 88.3% vs 83.9% at 4 y, and 85.5% vs 81.0% at 5 y (absolute improvement of 2.7%, 4.4%, and 4.5%, respectively). iDFS benefit was observed across subgroups, including N0 (HR, 0.606; 95% CI: 0.372-0.986). RIB + NSAI also demonstrated continued DDFS (HR, 0.709; 95% CI: 0.608-0.827) and DRFS (HR, 0.699; 95% CI: 0.594-0.824) benefit vs NSAI alone. A positive trend for OS favoring RIB + NSAI (HR, 0.800; 95% CI: 0.637-1.003; nominal 1-sided P=.026) continues to emerge. No new safety signals were observed with a median follow-up time of approximately 2 years after RIB completion.
Conclusions:
In this 5-year landmark analysis with mature efficacy data, RIB + NSAI reduced the risk of invasive and distant disease recurrence compared with NSAI alone, including in pts with high-risk N0 disease. A positive trend for OS in favor of RIB + NSAI continues to emerge.
An interview with: Javier C Cortés MD PhD, Breast Cancer Medical Oncologist, IOB Madrid, Institute of Oncology, Madrid, and International Breast Cancer Centre, Barcelona, Spain
BERLIN, Germany—Treatment with the antibody drug conjugate (ADC) sacituzumab govitecan (that targets the Trop-2 cancer-associated protein, delivering a cytotoxic topoisomerase inhibitor payload) has significantly improved progression-free survival in patients with newly-diagnosed metastatic triple-negative breast cancer who were not candidates for treatment with immune checkpoint inhibition and had received no prior therapy.
At the European Society for Medical Oncology (ESMO) 2025 Annual Congress Javier C Cortés MD PhD from the Institute of Oncology in Madrid and the International Breast Cancer Centre in Barcelona reported data from the ASCENT-03 study showing that treatment with sacituzumab govitecan brought clinically meaningful benefits with toxicities that were found to be manageable.
At the congress Cortés talked about the new findings with Peter Goodwin:
Audio Journal of Oncology: Javier C Cortes MD PhD
“[GOODWIN] Peter Goodwin here in Berlin …..……….Audio Journal of Oncology, I’m Peter Goodwin. 9:47secs
ESMO ABSTRACT:
LBA20 – “Primary results from ASCENT-03: A randomized phase III study of sacituzumab govitecan (SG) vs chemotherapy (chemo) in patients (pts) with previously untreated advanced triple-negative breast cancer (TNBC) who are unable to receive PD-(L)1 inhibitors (PD-[L]1i)”
Speaker: Javier C. Cortés (Barcelona, Spain)
Authors: Javier C. Cortés (Barcelona, Spain), Aditya Bardia (Los Angeles, United States of America), Kevin Punie (Antwerp, Belgium), Carlos H. Barrios (Porto Alegre, Brazil), Sara A. Hurvitz (Seattle, United States of America, CA),Andreas Schneeweiss (Heidelberg, Germany), Joohyuk Sohn (Seoul, Republic of Korea), Eriko Tokunaga (Fukuoka, Japan), Adam M. Brufsky (Pittsburgh, United States of America, PA), Yeon Hee Park (Seoul, Republic of Korea), Binghe Xu (Beijing, China), Roberto Hegg (São Paulo, Brazil), Mafalda Oliveira (Barcelona, Spain), Alessandra Fabi (Rome, Italy), Natalya Vaksman (Miami, United States of America), Theresa Valdez (Miami, United States of America), Xinrui Zhang (Miami, United States of America), Catherine Lai (Foster City, United States of America, CA), Sara M. Tolaney (Boston, United States of America, MA)
Background
Significant PFS benefit was observed with SG vs chemo in pretreated metastatic (m)TNBC (ASCENT) and with SG + pembrolizumab vs chemo + pembrolizumab in first-line (1L) PD-L1+ mTNBC (ASCENT-04). For pts with mTNBC who cannot receive PD-(L)1i, treatment options are limited. We report primary results from the randomized phase 3 ASCENT-03 study (NCT05382299) of 1L SG vs chemo in pts with locally advanced unresectable or mTNBC who are unable to receive a PD-(L)1i.
Methods
Pts had centrally confirmed PD-L1− mTNBC (defined as combined positive score [CPS] < 10) or PD-L1+ mTNBC (CPS ≥ 10) but were unable to receive PD-(L)1i due to a comorbidity or prior use in the curative setting. Randomization (1:1) to SG (10 mg/kg IV, days 1 & 8 in 21-day cycles) or chemo (paclitaxel, nab-paclitaxel, or gemcitabine + carboplatin) was stratified by disease status and geography. The primary end point was PFS by BICR. Key secondary end points included overall survival (OS), ORR and DOR by BICR, and safety.
Results
558 pts (279 in each group) with mTNBC were randomized. With a median follow-up of 13.2 mo, SG showed a significant improvement in median PFS vs chemo (9.7 vs 6.9 mo; HR, 0.62; 95% CI, 0.50-0.78; P < .0001); median DOR was 12.2 mo vs 7.2 mo (Table). OS data were immature. The most frequent grade ≥ 3 TEAEs were neutropenia (43%) and diarrhea (9%) with SG and neutropenia (41%) and anemia (16%) with chemo.
Conclusions
SG led to a statistically significant and clinically meaningful improvement in PFS and more durable responses vs chemo in 1L mTNBC. The safety profile of SG was manageable and consistent with its known profile; treatment discontinuation rate due to TEAEs was lower with SG vs chemo. These data support SG as a potential new standard of care for pts with previously untreated mTNBC who are unable to receive a PD-(L)1i. Table: LBA20
Clinical trial identification
NCT05382299.
Editorial acknowledgement
Editorial assistance was provided by Peggy Robinet, PharmD, PhD, and Sonal S. Joshi, PhD, of Parexel, and funded by Gilead Sciences, Inc.
Legal entity responsible for the study
Gilead Sciences, Inc.
Funding
Gilead Sciences, Inc.
PRESS RELEASE:
ASCENT-03: Trodelvy® Demonstrates Highly Statistically Significant & Clinically Meaningful Improvement in Progression Free Survival in Patients With First-line Metastatic Triple-Negative Breast Cancer Who Are Not Candidates for Checkpoint Inhibitors
– Second Positive Phase 3 Trial in First-line Metastatic TNBC Where Trodelvy Has Demonstrated a Clinically Meaningful Benefit Versus Standard of Care Chemotherapy –
– Trodelvy Has the Potential to Be the Backbone of Treatment and the First Antibody-Drug Conjugate for All Patients Across First-line Metastatic TNBC –
FOSTER CITY, Calif.–(BUSINESS WIRE)– Gilead Sciences, Inc. (Nasdaq: GILD) today announced positive topline results from the Phase 3 ASCENT-03 study of Trodelvy® (sacituzumab govitecan-hziy). The study met its primary endpoint, demonstrating a highly statistically significant and clinically meaningful improvement in progression-free survival (PFS) compared to chemotherapy in patients with first-line metastatic triple-negative breast cancer (mTNBC) who are not candidates for PD-1/PD-L1 inhibitors, meaning they are PD-L1 negative or are ineligible to receive immunotherapy.
“Almost half of the patients diagnosed with metastatic triple-negative breast cancer do not receive treatment beyond first-line, demonstrating an urgent need for innovative treatment options in this early setting,” said Dr. Javier Cortes, Head of the International Breast Cancer Center in Spain and principal investigator of the ASCENT-03 study. “Traditional chemotherapy has been the standard of care for early treatment of metastatic triple-negative breast cancer, and we know that therapeutic advances in this disease area serve a critical unmet need for patients and the broader oncology community.”
Together with the recently announced positive results from the ASCENT-04 study evaluating Trodelvy plus Keytruda® in patients with previously untreated PD-L1+ metastatic TNBC, Trodelvy now has the potential to be the backbone treatment for all patients across first-line mTNBC. Detailed data from the ASCENT-04 study will be shared during the American Society of Clinical Oncology (ASCO) meeting taking place May 30 – June 3, 2025.
“The ASCENT-03 outcome represents the first clinically meaningful advance for this patient population in over 20 years versus chemotherapy,” said Dietmar Berger, MD, PhD, Chief Medical Officer, Gilead Sciences. “By addressing this aggressive and difficult to treat disease earlier, we can potentially improve treatment options for the high unmet need that patients with metastatic triple-negative breast cancer face.”
The safety profile of Trodelvy in the ASCENT-03 study was consistent with prior studies, and no new safety signals were identified in this patient population. Overall survival (OS) is a key secondary endpoint and was not mature at the time of PFS primary analysis. No OS detriment was observed. Gilead will continue to monitor OS outcomes, with ongoing patient follow-up and further analysis planned.
Detailed results from the ASCENT-03 study will be presented at a future medical meeting and discussed with regulatory authorities. The use of Trodelvy in first-line mTNBC is investigational, and the safety and efficacy of this use have not been established.
Healthcare professionals have well-established experience with Trodelvy, which has shown generally consistent outcomes across both clinical trials and real-world studies in 60,000+ patients across 50+ countries over approximately five years. It is the only antibody-drug conjugate (ADC) with four positive Phase 3 trials in HER2- (IHC 0, IHC 1+ or IHC 2+/ISH–) metastatic breast cancer (mBC), and remains the only approved Trop-2-directed ADC that has demonstrated meaningful survival advantages in two different types of metastatic breast cancers: 2L mTNBC and pre-treated HR+/HER2- mBC.
Trodelvy is a Category 1 preferred treatment for both currently approved indications per the National Comprehensive Cancer Network® (NCCN®) Clinical Practice Guidelines in Oncology (NCCN Guidelinesi) and the only ADC with an ESMO Magnitude of Clinical Benefit Scale (MCBS) rating of 5 for mTNBC. Trodelvy also has an MCBS rating of 4 for women with HR+/HER2- mBC.
Currently, Gilead has additional ongoing Phase 3 studies investigating Trodelvy across HER2- (IHC 0, IHC 1+ or IHC 2+/ISH–) breast cancer including the ASCENT-07 pivotal trial in patients with HR+/HER2- mBC who have received endocrine therapy, and the ASCENT-05 pivotal trial in patients with early-stage TNBC (eTNBC). Trodelvy is also being evaluated in additional Phase 3 studies across a range of tumor types, including in lung and gynecologic cancers.
Gilead would like to thank the patients, families, investigators and advocates who have contributed and continue to contribute to this important research. We remain committed to advancing care to address the unmet needs for the breast cancer community.
KEYTRUDA® is a registered trademark of Merck Sharp & Dohme LLC., a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
About Triple-Negative Breast Cancer (In Patients Who Are Not Candidates for PD-1/PD-L1 inhibitors)
Triple-negative breast cancer (TNBC) is the most aggressive type of breast cancer and has historically been difficult to treat, accounting for approximately 15% of all breast cancers. TNBC disproportionately impacts younger, pre-menopausal as well as Black and Hispanic women. TNBC cells do not have estroge
An interview with:
Trevor Leong MD, Peter McCallum Cancer Centre, Radiation Oncology Department, Melbourne, Australia
BARCELONA, Spain—Although pre-operative radiotherapy brought better response rates in patients resected for their gastric or GE-junction adenocarcinomas, there was no improvement in survival. This is the clear finding from a big, long-term study led by an Australian team.
The multi-continent, phase-three randomized TOP GEAR trial, headquartered in Sydney Australia, definitively found no benefit for overall or progression-free survival from adding radiation before surgery.
This clear finding was announced at the 2024 Annual Meeting of the European Society for Medical Oncology (ESMO), held in Barcelona, Spain
First author Trevor Leong MD, from the Radiation Oncology Department of the Peter McCallum Cancer Centre in Melbourne Australia, talked about the results with Peter Goodwin:
Trevor Leong MD interview (8mins 37 secs):
IN: “Resectable gastric or gastro-esophageal…. OUT: ,,’till next time, Good-bye.”
ESMO 2024, Barcelona, ABSTRACT:
03880-8/fulltext
“A randomised phase three trial of perioperative chemotherapy (CT) with or without pre-operative chemoradiotherapy (CRT) for resectable gastric cancer (AGITG TOPGEAR). Final results from an intergroup trial of AGITG, TROG, EORTC and CCTG”.
NEJM September 13, 2024:
https://www.nejm.org/doi/full/10.1056/NEJMoa2405195
TITLE:
“Preoperative Chemoradiotherapy for Resectable Gastric Cancer”
From: The Australasian Gastro-Intestinal Trials Group, National Health and Medical Research Council Clinical Trials Centre, Trans-Tasman Radiation Oncology Group, European Organisation for Research and Treatment of Cancer, and Canadian Cancer Trials Group.
JOURNAL Article: N Engl. J Med.:
“The addition of preoperative chemoradiotherapy to perioperative chemotherapy did not improve overall survival as compared with perioperative chemotherapy alone among patients with resectable gastric and gastroesophageal junction adenocarcinoma.”
“A randomised phase three trial of perioperative chemotherapy (CT) with or without pre-operative chemoradiotherapy (CRT) for resectable gastric cancer (AGITG TOPGEAR). Final results from an intergroup trial of AGITG, TROG, EORTC and CCTG”.
Background
In Western countries, the current standard of care for resectable gastric cancer is periop CT. There is much interest in preop CRT, but comparison to periop CT alone is lacking. In TOPGEAR we hypothesized that adding preop CRT to periop CT would improve pathological complete response (pCR) rates and ultimately overall survival (OS) compared to periop CT alone.
Methods
This international phase 3 trial randomized patients with resectable adenocarcinoma of the stomach and gastro-esophageal junction to periop CT alone, or with preop CRT. The periop CT alone group received 3 cycles of epirubicin/cisplatin/5-fluorouracil (ECF) or 4 cycles of fluorouracil/leucovorin/oxaliplatin/docetaxel (FLOT) both pre- and post-operatively. The preop CRT group received one less cycle of preop chemotherapy followed by chemoradiotherapy (45 Gy in 25 fractions radiation plus infusional 5-FU ), and then the same postop chemotherapy. The primary endpoint was overall survival, and secondary endpoints included progression free survival (PFS), pCR rates, toxicity and quality of life.
Results
Between September 2009 and May 2021, 574 patients were enrolled from 70 sites across 15 countries in Australasia, Europe, and Canada; 288 to periop CT group and 286 to preop CRT group. Compared to periop CT alone, patients receiving preop CRT achieved a higher pCR rate (16.7% vs 8.0%), a higher rate of major pathological response (0 – <10% residual tumor: 49.5% vs 29.3%), and greater tumor downstaging following resection. After a median follow-up of 66.7 months, there was no significant difference in OS or PFS: median OS periop CT 49.4 months vs preop CRT 46.4 months; median PFS periop CT 31.8 months vs preop CRT 31.4 months. Preop CRT was not associated with increased perioperative treatment toxicity or a higher rate of surgical complications.
Conclusions
Despite improving pathological outcomes, the addition of preop CRT to periop CT does not improve overall survival compared to periop CT alone in patients with resectable gastric and gastro-esophageal junction adenocarcinoma.
Clinical trial identification
ACTRN12609000035224. Registered 30 May 2009; NCT01924819.
Legal entity responsible for the study
Australasian Gastro-Intestinal Trials Group (AGITG).
Funding
This work was supported by grants from the National Health and Medical Research Council: 1046425 and 2000711, Canadian Institutes of Health Research (CIHR) grant no. 119445, the Canadian Cancer Society Research Institute (CCSRI) grant no. 021039, the Health Research Council of New Zealand (HRC) International Investment Opportunities Fund: Contract no. 09/624, the EORTC Cancer Research Fund, and the Cancer Australia Priority-driven Collaborative Research Scheme: Project ID: 570996.
Disclosure
K.M. Haustermans: Financial Interests, Personal, Other, Clinical editor Radiotherapy & Oncology: Elsevier; Financial Interests, Institutional, Funding: IBA; Financial Interests, Institutional, Research Grant: Varian,
https://www.audiomedica.com/wp-content/2025/10/Trevor-Leong-ESMO-AJO-PRODUCTION-MASTER.mp3Editorial acknowledgement
Editorial and medical writing support was provided in accordance with Good Publication Practice guidelines by Lewis Cawkwell, PhD, of Parexel, and was funded by AstraZeneca.
Legal entity responsible for the study
AstraZeneca.
An interview with: Domenica Lorusso MD PhD, Director of the Gynaecological Oncology Unit, full Professor of Obstetrics and Gynaecology, Humanitas Hospital San Pio X, Fondazione Policlinico Universitario A. Gemelli IRCCS, Catholic University of the Sacred Heart, Rome, Italy.
Both overall and progression-free survival were significantly improved when the anti-PD-1 agent pembrolizumab was added to standard chemoradiotherapy as initial treatment for patients with high-risk locally advanced cervical cancer.
Results from the randomized, double-blind, phase III KEYNOTE-A18 study of immunotherapy, used together with standard concurrent chemoradiotherapy among 1060 patients, were reported by a multinational team of researchers led from Italy to the 2024 Annual Congress of the European Society for Medical Oncology in Barcelona.
The study lead author Domenica Lorusso MD PhD, Director of the Gynaecological Oncology Unit at Humanitas Hospital San Pio X, in Milan, who is a Full Professor of Obstetrics and Gynaecology at Humanitas University, Rozzano, met up with Peter Goodwin to discuss the KEYNOTE-A18 findings.
Audio Journal of Onclogy: Domenica Lorusso MD PhD IN: “Immune checkpoint inhibition …..OUT: …….in Barcelona at the ESMO meeting”. Durn: 7:20 secs
ESMO Abstract 7090
Lorusso, Gynaecology Oncology Unit, Fondazione Policlinico Universitario A. Gemelli IRCCS and Catholic University of the Sacred Heart, Rome, Italy
“Pembrolizumab plus chemoradiotherapy for high-risk locally advanced cervical cancer: Overall survival results from the randomized, double-blind, phase III ENGOT-cx11/ GOG-3047/KEYNOTE-A18 study”
Background
At the first interim analysis of the phase 3 ENGOT-cx11/GOG-3047/KEYNOTE-A18 study (NCT04221945), pembrolizumab (pembro) + concurrent chemoradiotherapy (CCRT) showed a statistically significant and clinically meaningful improvement in PFS vs placebo (pbo) + CCRT in patients (pts) with high-risk locally advanced cervical cancer (LACC). Based on this study, the US FDA has approved pembro + CCRT for pts with FIGO 2014 Stage III-IVA cervical cancer. We present the OS results from the second interim analysis.Methods
Eligible pts with newly diagnosed, previously untreated, high-risk LACC (FIGO 2014 stage IB2-IIB with node-positive disease or stage III-IVA regardless of lymph node status) were randomized 1:1 to 5 cycles of pembro 200 mg or pbo Q3W + CCRT, then 15 cycles of pembro 400 mg or pbo Q6W. CCRT included 5 cycles (optional 6th dose) of cisplatin 40 mg/m2 Q1W + EBRT then brachytherapy. Pts were stratified by planned EBRT type (intensity-modulated radiotherapy [IMRT] or volumetric-modulated arc therapy [VMAT] vs non-IMRT or non-VMAT), stage at screening (IB2-IIB vs III-IVA), and planned total radiotherapy dose (<70 Gy vs ≥70 Gy [EQ2D]). Primary endpoints are PFS per RECIST v1.1 by investigator and OS.Results
1060 pts were randomized to pembro + CCRT (n=529) or pbo + CCRT (n=531). At this analysis (January 8, 2024, data cutoff), median follow-up was 29.9 mo (range, 12.8-43.0). Pembro + CCRT showed a statistically significant improvement in OS compared with pbo + CCRT. The 36-mo OS rate was 82.6% with pembro + CCRT vs 74.8% with pbo + CCRT; median OS was NR in either group (HR=0.67 [95% CI, 0.50-0.90]; P=0.0040). The benefit of pembro + CCRT was generally consistent in all prespecified subgroups, including FIGO stages IB2-IIB (HR=0.89 [95% CI, 0.55-1.44]) and III-IVA (HR=0.57 [95% CI, 0.39-0.83]). Grade ≥3 TRAE incidence was 69.1% in the pembro + CCRT group and 61.3% in the pbo + CCRT group.
Conclusions
Pembro + CCRT showed a statistically significant and clinically meaningful improvement in OS vs pbo + CCRT in pts with high-risk LACC and had a manageable safety profile. These data provide further support for pembro + CCRT as a new standard of care for this population.
Clinical trial identification
NCT04221945; EudraCT: 2019-003152-37.
Editorial acknowledgement
Medical writing assistance was provided by Christine McCrary Sisk of Merck & Co., Inc., Rahway, NJ, USA. This assistance was funded by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ,
Audio Journal of Oncology, October 6, 2025
An interview with:
James Larkin FRCP, PhD, Medical Oncologist, Professor, Royal Marsden Hospital, London
Checkpoint inhibitor therapy for advanced melanoma has achieved sustained responses and long-term overall survival, transforming the prognosis for as many as half of all patients. 10-year survival outcomes from the phase Ill CheckMate 067 trial of nivolumab plus ipilimumab in advanced melanoma were reported at the 2024 Annual Meeting of the European Society for Medical Oncology (ESMO) held in Barcelona.
Peter Goodwin, talked with study author, James Larkin FRCP PhD, Professor and Medical Oncologist at the Royal Marsden Hospital in London.
Audio Journal of Oncology: James Larkin FRCP PhD: IN: “There’s been breath-taking progress ………OUT: join me then, Good-bye!” 14:57secs
SOURCE:
Annals of Oncology:
https://www.annalsofoncology.org/article/S0923-7534(24)03864-X/fulltext
ESMO Abstract LBA43
Larkin, Medicine Department, The Royal Marsden Hospital, London, UK
“10-y survival outcomes from the phase Ill CheckMate 067 trial of nivolumab plus ipilimumab in advanced melanoma”
Abstract LBA43
Larkin, Medicine Department, The Royal Marsden Hospital, London, UK
“10-y survival outcomes from the phase Ill CheckMate 067 trial of nivolumab plus ipilimumab in advanced melanoma”
Background
In CheckMate 067, improved survival with nivolumab plus ipilimumab (NIVO + IPI) or NIVO alone v IPI has been demonstrated in patients (pts) with advanced melanoma. We now provide the final CheckMate 067 results (minimum f/u 10 y), the longest reported in a phase 3 study of an anti–programmed death (PD)-1–based therapy for any tumor type.
Methods
Pts with untreated advanced melanoma (N = 945) were randomly assigned 1:1:1 and stratified by PD-ligand (L)1 status, BRAF mutation status, and metastasis stage to receive NIVO (1 mg/kg) + IPI (3 mg/kg) Q3W for 4 doses, followed by NIVO (3 mg/kg) Q2W; NIVO (3 mg/kg) Q2W + placebo; or IPI (3 mg/kg) Q3W for 4 doses + placebo until progression or unacceptable toxicity. Co-primary endpoints were OS and PFS with NIVO + IPI or NIVO v IPI; melanoma-specific survival (MSS) was an exploratory endpoint.
Results
After a 10-y minimum f/u, median OS was 71.9 mo with NIVO + IPI, 36.9 mo with NIVO, and 19.9 mo with IPI. OS HRs were 0.53 (95% CI, 0.44–0.65) with NIVO + IPI vIPI and 0.63 (0.52–0.76) for NIVO v IPI, and benefit was consistent across subgroups (including PD-L1 expression and BRAF mutation status). Median MSS was not reached (NR) with NIVO + IPI (> 120 mo), 49.4 mo with NIVO, and 21.9 mo with IPI. In pts who had PFS for ≥ 3 y, 10-y MSS rates were 96% with NIVO + IPI, 97% with NIVO, and 88% with IPI. Only 8 pts, 4 in the NIVO + IPI arm and 4 in the NIVO arm, progressed beyond 60-mo of f/u. For pts in the NIVO + IPI arm who discontinued treatment during induction due to a treatment-related adverse event, 10-y OS rates were the same as the ITT group (43%) and MSS rates were similar (50% v 52%). Table: LBA43”
MORE:
James Larkin is a Medical Oncologist specialising in the treatment of cancers of the kidney and skin including melanoma.
Professor Larkin grew up in North Cornwall before taking a first in Natural Sciences from Cambridge University. He undertook clinical training in Oxford, qualifying in 1996. His general medical training was undertaken in London and in 2001 he won a Medical Research Council Research Fellowship for a Clinician, carrying out laboratory research leading to a PhD at the Institute of Cancer Research. His specialist training was completed at The Royal Marsden, where he was appointed as a Consultant in 2008.
His research is focussed on trying to understand cancer and its consequences better, as well as developing improved treatments, particularly with targeted therapies and immunotherapies. Globally, he is amongst the most highly cited researchers in both melanoma and kidney cancerThis link is external and opens in a new tab.
In 2018, he was elected as a Fellow of the Academy of Medical Sciences and in 2020 as an NIHR Senior Investigator. In 2022, he was appointed to roles as Head of The Royal Marsden Skin Unit, Royal Marsden Joint Training Programme Director for Medical Oncology and Lead of the Cancer Immunotherapy Theme at The Royal Marsden / Institute of Cancer Research NIHR Biomedical Research Centre.
Since 2024, he has hosted the educational podcast ‘Melanoma Matters’ with his US colleague Professor Sapna Patel, and in 2026 he will be Scientific Co-Chair of the Annual European Society of Medical Oncology meeting in Madrid.
Professor Larkin serves as a medical advisor to the patient advocacy group Melanoma UK, as a trustee of Action Kidney Cancer and sits on the Medical Advisory Board of the International Kidney Cancer Coalition.
An interview with: Jefferson DeKloe BSc, Department of Otolaryngology, Thomas Jefferson University, Philadelphia, PA
CHICAGO, USA—Although the take-up of vaccination for human papilloma virus (HPV) among girls and boys in the USA has been lower than in many other industrial countries, American researchers have now shown clearly that in addition to the prevention of cervical cancer in women, men have also been protected against HPV-related cancers.
At the 2024 American Society of Clinical Oncology Annual (ASCO) Meeting in Chicago a new study of HPV vaccination of girls and boys in the United States revealed a real-world reduction of oral, plus head and neck cancers in men, as well confirming the prevention of cervical cancers in women, even though uptake of the vaccine in the US had been sub-optimal. The study looked at HPV-associated cancer incidence in a retrospective cohort analysis of patients from the TriNetX Collaborative Network.
At the ASACO meeting Peter Goodwin met up with the lead author of the research, Jefferson DeKloe BSc, from the Department of Otolaryngology at Thomas Jefferson University in Philadelphia USA.
Audio Journal of Oncology, with: Jefferson DeKloe BSc
IN: “HPV Vaccination …..OUT: ……, I’m Peter Goodwin”. 6:00secs
https://meetings.asco.org/abstracts-presentations/231759
“Effects of HPV vaccination on the development of HPV-related cancers: A retrospective analysis of a United States-based cohort.”
https://ascopubs.org/doi/10.1200/JCO.2024.42.16_suppl.10507
Effects of HPV vaccination on the development of HPV-related cancers: A retrospective analysis of a United States-based cohort.
ALSO:
https://www.sciencedirect.com/science/article/pii/S1043661825002762
HPV vaccination and malignancy risks beyond cervical cancer: A retrospective global cohort study
Authors: Christian Seebauer, Mohamed Faluogy, Peter Sieg , Henning Olbrich, Ralf Ludwig
Department of Oral and Maxillofacial Surgery/Plastic surgery, University Medicine Lübeck, Ratzeburger Allee 160, Lübeck 23538, Germany
Department of Dermatology, Allergy, and Venerology, University of Lübeck, Ratzeburger Allee 160, Lübeck 23538, Germany
Department of Dermatology, Allergy, and Venerology, Institute of Experimental Dermatology, University of Lübeck, Comprehensive Center for Inflammation Medicine, University-Hospital Schleswig-Holstein, Ratzeburger Allee 160, Lübeck 23538, Germany
Received 28 April 2025, Revised 5 July 2025, Accepted 6 July 2025, Available online 11 July 2025, Version of Record 14 July 2025.
HPV vaccination significantly reduced hypopharyngeal and laryngeal cancer risk.
Vaccination was associated with a marked decrease in leukemia incidence.
No significant protection observed for rectal, anal, or oral cavity cancers.
HPV vaccination halved all-cause mortality at 8- and 20-year follow-up.
Data support possible HPV involvement in hematopoietic and neuronal tissues.
Abstract:
While HPV vaccination is well established for the prevention of cervical cancer, its broader oncological effects remain insufficiently characterized. Emerging evidence suggests potential protective effects against non-cervical malignancies; however, comprehensive long-term data are limited. We conducted a global, retrospective cohort study utilizing electronic health records from the TriNetX network. Individuals vaccinated against HPV at age 8 years or older were propensity score-matched to unvaccinated controls. Outcomes included the incidence of malignancies in the head-and-neck, gastrointestinal, anogenital, neuronal, and hematologic systems, as well as all-cause mortality, assessed over 8- and 20-year follow-up periods. Kaplan–Meier survival analysis and hazard ratios (HRs) were employed. HPV vaccination was associated with significant reductions in the risk of hypopharyngeal and laryngeal carcinomas (8-year HR: 0.19; 95 % CI: 0.057–0.631; p = 0.0025; 20-year HR: 0.227; 95 % CI: 0.067–0.764; p = 0.0092) and leukemia (8-year HR: 0.461; p = 0.0035; 20-year HR: 0.443; p = 0.0019). No significant protection was observed for rectal, anal, oral cavity, or prostate cancers. All-cause mortality was reduced by nearly half among vaccinated individuals (8-year HR: 0.543; 20-year HR: 0.536; both p < 0.0001). Beyond epithelial malignancies, HPV vaccination may confer systemic cancer protection, particularly in hematologic and potentially neuronal tissues. These findings suggest a broader biological impact of HPV vaccination than previously recognized and underscore the need for mechanistic studies investigating HPV’s oncogenic pathways. If validated, these results could prompt the expansion of vaccination strategies to encompass broader indications and wider population coverage.
An interview with Rebecca Dent MD, Deputy Chief Executive Officer, National Cancer Centre, Singapore, ESMO 2024 Scientific Chair.
ESMO Previous Highlights: Neo-Adjuvant Therapy for Triple Negative Breast Cancer, Checkpoint Inhibition, AI, Cancer Vaccines, and More ……”
BARCELONA, Spain—At the last Annual Meeting of the European Society for Medical Oncology (ESMO), medical oncologist Rebecca Dent MD, Deputy Chief Executive Officer at the National Cancer Centre in Singapore, told Peter Goodwin what had, for her, been the key areas of progress in cancer medicine announced at the meeting in which significant advances had been made.
Audio Journal of Oncology with Rebecca Dent MD IN: [Goodwin] “With the 2025 meeting of ESMO about to happen …. OUT: ….in Singapore. Thanks very much. 13:13 secs
https://www.esmo.org/meeting-calendar/esmo-congress-2024/programme
MORE:
Professor Rebecca Dent MD MSc is a career-long clinical and translational researcher as well as education-focused, academic clinician with sub-specialist interest in all aspects of triple negative breast cancer (TNBC) and young women with breast cancer.
Prof. Dent achieved her MD from McMaster University in Hamilton, Ontario, Canada and then completed her internal medicine and medical oncology residency at the Princess Margaret Hospital and the Sunnybrook Odette Cancer Center in Toronto, Canada. This was followed by a fellowship in breast cancer, supported by a Marion Walker Women’s Health Scholarship, and MSc in Clinical Epidemiology and Statistics at the University of Toronto. During her training Prof Dent was fortunate to have completed electives across Canada, the US (Memorial Sloan Kettering), France (Institut Marie Curie) and the Philippines (Philippine General Hospital).
In her North American academic career, Prof Dent served as Chair of the locally advanced breast cancer program and Head, Breast Cancer Clinical Trials Unit at the Sunnybrook Odette Cancer Center from 2008-2011. Her seminal publication whilst in Toronto was a Clinical Cancer Research publication, one of the first to describe what is now known as triple negative with almost 5,500 citations for this individual paper (Dent R et al. Clin Ca Res 2007). She was the PI of one of the first Phase I PARP inhibitor trials in unselected TNBC in combination with taxane chemotherapy and she served as a reviewer for the National Cancer Institute of Canada (NCIC) grants committee. As a consultant at the Sunnybrook Odette Cancer Center, she supervised a number of residents and fellows and was awarded an Outstanding Teaching Award by the University of Toronto.
Prof Dent has participated in the ASCO Leadership Development Program and served on a number of ASCO Committees: Education including Chair, Breast Track and Member of the Breast Scientific Committee (ER/HER2 track), as well as on the Editorial Board of the Journal of Clinical Oncology (JCO).
In February 2011, Prof Dent moved to Singapore where she is now senior consultant at the National Cancer Center in Singapore (NCCS). Recognizing the need for pan-Asian regional educational interaction Prof Dent co-founded and co-chaired nine Asia Pacific Breast Cancer Summits (https://apbcs.org). Consequently Prof Dent was involved in the establishment of the ESMO Asia meeting subsequently serving as Scientific Chair and Co-Chair Breast Track. Prof Dent has co-chaired the ESMO Breast Preceptorship in Singapore since 2017 and sits on the pan-Asian ESMO adapted guidelines committee as well as the Advanced Breast Cancer ESMO guideline committee. Prof Dent serves as a scientific committee member of the ASCO Breakthrough Asia Meeting. Prof Dent is currently Chair of the ESMO Nomination Committee and a member of the ESMO Council.
Prof Rebecca Dent has over 18,000 citations and an h-index over 50. She sits on the Editorial Board of The Lancet Oncology. She has been invited as an oral and plenary discussant at ESMO as well as an invited speaker at numerous meetings for ASCO, ESMO Asia, and other meetings across Asia such as the Japanese Society of Medical Oncology and Korean Society of Medical Oncology. Prof Dent is a steering committee member and PI for a number of large international trials evaluating novel agents in the treatment of TNBC. Funding was secured for a novel investigator initiated global study evaluating the role of PARP inhibition with or without immune checkpoint inhibition in platinum sensitive TNBC which has just completed recruitment in the US, Korea and in Singapore (The DORA study). This is a pivotal Duke NUS Singapore and Duke USA collaboration.
As of October 2018, Prof Dent has been Head of the department of Medical Oncology at the National Cancer Center Singapore (NCCS) at SingHealth. NCCS has recently been designated as a comprehensive cancer center and Prof Dent was appointed Chairman of the Division of Medical Oncology in 2021.
Prof Dent maintains a busy clinical practice, as well as teaching medical students at Duke-NUS. This has been recognized with a star award for Quality National Service and the SingHealth Outstanding Clinician Award. Most recently in 2023 she was one of the Singapore National Health Quality Service Superstar award winners.