Discover Nick Sterling, MD, PhD
Nick Sterling, MD, PhD

20 Episodes
Reverse
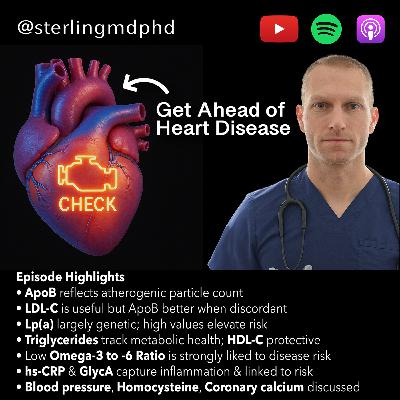
In this episode, we cover why early atherosclerosis is essentially universal by young adulthood and tests that tell us about cardiovascular risk—beyond a standard lipid panel. We walk through ApoB (and why it can outperform LDL-C in some circumstances), Lp(a) and the case for checking it at least once, inflammation markers like hs-CRP and GlycA, the triglyceride–HDL relationship and TG/HDL ratio, omega-3:omega-6 balance (including an important atrial fibrillation caveat), blood pressure and endothelial stress, plus quick thoughts on homocysteine and coronary calcium scoring.Chapters:00:00 — Why almost everyone has early plaque00:01:01 — ApoB explained 00:02:12 — ApoB vs LDL-C: discordance00:02:38 — Lp(a)00:04:34 — Inflammation: hs-CRP & GlycA00:05:44 — Triglycerides & HDL00:07:19 — Omega-3:6 ratio & Atrial Fibrillation caution00:08:14 — Blood pressure & endothelial stress00:10:03 — Homocysteine & CACSpotify Channel:https://podcasters.spotify.com/pod/show/sterlingmdphd/Social & Website:Instagram - https://www.instagram.com/sterlingmdphdX - https://x.com/sterlingmdphdFacebook - / sterlingmdphdNewsletter - http://eepurl.com/hQpdqTApple Podcasts: https://apple.co/3y438C9References & Show Notes:http://www.nicksterling.com/This content is not medical advice, is for general information purposes only and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. This content is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit http://nicksterling.com/terms for full Terms of Use.
Spotting Metabolic Dysfunction Early: LP-IR, Waist-to-Hip, Uric Acid & More. In this episode, we cover practical ways to spot early metabolic dysfunction. We walk through the LP-IR (lipoprotein insulin resistance) index and what changing lipid particle patterns reveal, then show how to measure waist-to-hip ratio correctly and interpret risk thresholds. We also touch on where magnesium fits (and its small effects on blood pressure), how to read kidney function more accurately by pairing creatinine with cystatin C, what rising uric acid can signal (including ties to fructose intake and blood pressure), and simple lab/imaging clues of hepatic steatosis/NAFLD.HighlightsLP-IR flags insulin resistance before glucose markers shift.Waist-to-hip ratio is a strong visceral fat proxy.Creatinine + cystatin C improves eGFR accuracy.Uric acid links fructose intake to higher blood pressure.Chapter Markers00:00 Intro: avoid health “icebergs”00:00:41 Metabolic dysfunction 10100:01:26 LP-IR (lipoprotein insulin resistance) explained00:02:22 Triglycerides, VLDL & HDL in insulin resistance00:03:28 Small dense LDL & LP-IR00:04:51 Waist-to-hip ratio: measure & cutoffs00:06:14 Magnesium: insulin sensitivity & small BP effects00:06:47 Kidney function: creatinine + cystatin C (combined eGFR)00:09:06 Uric acid, fructose & blood pressure00:11:08 Liver fat (NAFLD): labs & imagingSpotify Channel:https://podcasters.spotify.com/pod/show/sterlingmdphd/Social & Website:Instagram - https://www.instagram.com/sterlingmdphdX - https://x.com/sterlingmdphdFacebook - / sterlingmdphdNewsletter - http://eepurl.com/hQpdqTApple Podcasts: https://apple.co/3y438C9References & Show Notes:http://www.nicksterling.com/This content is not medical advice, is for general information purposes only,and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. This content is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit http://nicksterling.com/terms for full Terms of Use.
In this episode, we cover the highest-yield lab tests to spot insulin resistance early—often years before routine screening would. I walk through how insulin works, why insulin resistance can be silent for a decade, and which metrics actually move the needle for long-term metabolic health.We dig into fasting glucose and A1C, fasting insulin, and combined indices like HOMA-IR and QUICKI. I also explain when an oral glucose tolerance test or a continuous glucose monitor can add value, the limitations of single time-point labs, and why calibration matters for CGMs. Finally, I preview how lipid test — particularly triglyceride-to-HDL ratio—can flag insulin resistance.Chapter Markers00:00 — Intro00:28 — Insulin resistance as a foundation01:11 — Common causes of mortality in U.S.02:07 — What insulin does (and what goes wrong)02:57 — Glucose tests: fasting glucose & A1C basics04:20 — Early signal: fasting insulin (typical ranges)05:16 — Combined indices: HOMA-IR & QUICKI (cutoffs & caveats)06:18 — OGTT & CGM07:31 — Continuous glucose monitor caveats09:10 — TG/HDL ratio for insulin resistanceHOMA-IR Calculatorhttps://www.mdcalc.com/calc/3120/homa-ir-homeostatic-model-assessment-insulin-resistanceQUICKI Calculatorhttps://www.mdapp.co/insulin-sensitivity-quicki-calculator-324/Quick Referencehttps://nicksterling.com/2025/09/18/quick-reference-guide-tests-for-insulin-resistance-part-1/Spotify Channel:https://podcasters.spotify.com/pod/show/sterlingmdphd/Social & Website:Instagram - https://www.instagram.com/sterlingmdphdX - https://x.com/sterlingmdphdNewsletter - http://eepurl.com/hQpdqTApple Podcasts: https://apple.co/3y438C9This content is not medical advice, is for general information purposes only,and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. This content is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit http://nicksterling.com/terms for full Terms of Use.
Scientific knowledge of the gut microbiome has increased exponentially over the last decade. Recently, several studies have suggested that specific strains of bacteria, including Akkermansia muciniphila, are key to supporting the environmental conditions required for other related bacterial strains that facilitate healthy metabolic health. In this video, Colleen Cutcliffe, PhD, co-founder and CEO of Pendulum discusses groundbreaking research around Akkermansia mucinophila, the role of short-chain fatty acids (SCFAs) in stimulating GLP-1 pathways, implications for diabetes management, and how gut bacteria influence inflammation, gut integrity, and overall metabolic health. They also explore how diet, antibiotics, and stress impact the microbiome, potential roles of probiotics in inflammatory bowel disease (IBD), pediatric gut health, and exciting emerging research on the gut-brain axis and neurological conditions like Parkinson's disease. Colleen highlights Pendulum's rigorous scientific approach, including clinical trials and innovative manufacturing practices that ensure product viability and effectiveness.Promotional code STERLING20 can be applied for 20% off of first membership purchases (https://pendulumlife.com). Please note that Dr. Sterling has no financial affiliation with Pendulum. This code is provided only as a discount to listeners and does not constitute a clinical recommendation or medical advice.Chapters:- 00:00 Intro: Gut Microbiome Essentials- 02:03 Pendulum's Biotech Innovation- 06:15 GLP-1 & Metabolic Health- 09:59 Probiotic Industry Insights- 17:17 Importance of Akkermansia- 24:17 Clinical Results for Diabetes- 29:28 Manufacturing Challenges- 39:13 Diet's Impact on Microbiome- 43:35 Gut-Brain Connection- 46:50 Next Steps & ResourcesSpotify Channel:https://podcasters.spotify.com/pod/show/sterlingmdphd/Social & Website:Instagram - https://www.instagram.com/sterlingmdphdX - https://x.com/sterlingmdphdNewsletter - http://eepurl.com/hQpdqTApple Podcasts: https://apple.co/3y438C9References & Show Notes:http://www.nicksterling.com/This content is not medical advice, is for general information purposes only and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. This content is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit http://nicksterling.com/terms for full Terms of Use.
Insulin resistance is a major risk factor for conditions like heart disease, stroke, and diabetes, yet its causes are not always well understood. This video explores the role of magnesium deficiency in insulin resistance and metabolic dysfunction, highlighting its impact on glucose metabolism, insulin signaling, and pancreatic function. We discuss how common magnesium deficiency is, why standard blood tests may not detect it, and who is at higher risk. Additionally, we review clinical evidence, including meta-analyses of randomized controlled trials, showing that magnesium supplementation can improve insulin sensitivity and glycemic control. Finally, we compare different forms of magnesium supplements, their absorption rates, and potential side effects.Spotify Channel:https://podcasters.spotify.com/pod/show/sterlingmdphd/Chapters:00:00 - Insulin Resistance & Health Risks00:19 - Reversible Cause of Insulin Resistance00:46 - Magnesium & Glucose Metabolism01:25 - Detecting Magnesium Deficiency02:07 - Risk of Magnesium Deficiency02:57 - How Magnesium Affects Insulin & Glucose04:16 - Key Mechanisms Explained06:08 - Clinical RCT Evidence & Studies08:27 - Magnesium Improves Blood Pressure09:05 - Organic & Inorganic Magnesium Supplements10:31 - Supplement Risks11:06 - Final Thoughts & SummarySocial & Website:Instagram - https://www.instagram.com/sterlingmdphdX - https://x.com/sterlingmdphdFacebook - / sterlingmdphdNewsletter - http://eepurl.com/hQpdqTApple Podcasts: https://apple.co/3y438C9References & Show Notes:http://www.nicksterling.com/This content is not medical advice, is for general information purposes only,and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. This content is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit http://nicksterling.com/terms for full Terms of Use.
What are some common side effects of medications like Ozempic and Wegovy? From the front lines of healthcare, we explore adverse effects of these medications based on real-world visits to the emergency department. Learn about common side effects such as nausea, dehydration, and muscle wasting, as well as lesser-known risks like starvation ketosis and mood changes.
Chapters
0:00 - Introduction to & GLP-1 RAs
0:48 - Nausea and Vomiting as Side Effects
1:52 - Dehydration Leading to Kidney Injury
3:11 - GLP-1 RAs & Starvation Ketosis
4:16 - Muscle Wasting on GLP-1 RAs
5:08 - Depression and Mood Changes
5:39 - Honorable Mention: Gastroparesis
Video on Muscle Wasting & GLP-1 Receptor Agonists:
https://youtu.be/Po2gC3zG0C8
Spotify Channel:
https://podcasters.spotify.com/pod/show/sterlingmdphd/
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Apple Podcasts: https://apple.co/3y438C9
References & Show Notes:
http://www.nicksterling.com/
This content is not medical advice, is for general information purposes only and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. This content is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit http://nicksterling.com/terms for full Terms of Use.
In this episode, we explore how ketamine, a dissociative anesthetic with a long history in medical use, is now being investigated for its rapid and sustained effects on depression, anxiety, and PTSD. We discuss its role in promoting neuroplasticity—rewiring the brain's structure to counteract stress-induced atrophy—and review the evidence from clinical trials, including a landmark 2023 meta-analysis. While ketamine shows promise in alleviating depressive symptoms and supporting neural growth, we also address its risks and the importance of professional oversight. Learn how this cutting-edge research is reshaping mental health treatment and what it means for the future of therapy.
Spotify Channel:
https://podcasters.spotify.com/pod/show/sterlingmdphd/#mentalhealth
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
X - https://x.com/sterlingmdphd
Facebook - / sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Apple Podcasts: https://apple.co/3y438C9
References & Show Notes:
http://www.nicksterling.com/
This content is not medical advice, is for general information purposes only,
and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. This content is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
Timestamps
00:00:00 - Depression Treatments and Challenges
00:00:20 - Brain Rewiring and Neuroplasticity
00:00:36 - Ketamine: A Rapid Neuroplasticity Tool
00:00:52 - Ketamine's Origins as an Anesthetic
00:01:28 - How Ketamine Works in the Brain
00:01:49 - Evidence of Ketamine's Effectiveness for Depression
00:03:04 - Human Trials and Clinical Findings
00:04:14 - Short-Term and Medium-Term Efficacy
00:04:31 - Exploring Ketamine for PTSD and Anxiety
00:05:54 - Brain Changes in Depression
00:08:50 - How Ketamine Reverses Brain Damage
00:10:02 - Ketamine's Neuroplasticity Mechanisms
00:12:11 - Risks and Side Effects of Ketamine Treatment
00:14:15 - Long-Term Concerns and Cognitive Impacts
00:15:05 - A Holistic Approach to Depression Management
00:15:22 - Thanks and Channel Support
In this episode, we talk about a recent study from Nature Aging that suggests aging may not progress in a straight line. Using data from thousands of biological measurements, researchers identified key ages—44 and 60—where changes in aging appear to accelerate. We review what this means for our understanding of aging, how it affects multiple systems in the body, and the potential implications for health and disease. We also discuss what this study tells us—and doesn’t tell us—about the biology of aging and how it could guide future research.
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://x.com/sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Apple Podcasts: https://apple.co/3y438C9
References & Show Notes: http://www.nicksterling.com/
The content of this podcast is not medical advice, is for general information purposes only, and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. The content of this podcast is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
Can we slow the speed of aging? In this episode, Dr. Varun Dwaraka, Head of Bioinformatics at TruDiagnostic, walks us through through the science of measuring "biological age" using epigenetic markers, such as DNA methylation. We discuss how epigenetics (i.e. DNA methylation), may provide biomarkers of biological age, the rate at which aging occurs, and potentially early markers of disease. Dr. Dwaraka explains the distinctions between chronological and biological age, the development and refinement of epigenetic clocks, and the potential applications of these tools in aging interventions. The conversation also addresses the mechanisms of epigenetic regulation, the influence of lifestyle factors on biological age, and the future role of epigenetics in predicting and managing age-related diseases. Additionally, we examine the data science that underpins these clocks, their targeted outcomes, and a recent study published by Dr. Dwaraka and colleagues comparing aging biomarker outcomes in a vegan vs. omnivore diet intervention among twins.
Chapters:
00:00 - Biological Age & Epigenetics
01:07 - What is Biological Age?
03:34 - Rate of Aging (aka. Speed of Aging)
05:28 - Epigenetics and Aging
11:14 - How the Epigenome Changes Over Time
18:26 - The Evolution of Epigenetic Clocks
24:49 - Understanding the Horvath Clock
30:03 - New Generations of Aging Clocks
34:07 - The Impact of Lifestyle on Biological Age
42:13 - The Future of Epigenetics in Predicting Disease
50:34 - Practical Applications of Epigenetic Testing
57:43 - The Role of Multi-Omics in Understanding Aging
01:07:34 - The Rejuvenation Olympics and the Future of Anti-Aging
Social & Website:
Instagram - / sterlingmdphd
Twitter - / sterlingmdphd
Facebook - / sterlingmdphd
TikTok - / sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F...
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
The content of this podcast is not medical advice, is for general information purposes only, and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. The content of this podcast is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
Why do humans get cardiovascular disease and how can we prevent it? These are critical processes to understand for anyone who is interested in living a longer and healthier life. I'm very honored to talk with Dr. Tom Dayspring, a world-renowned clinical lipidologist and physician whose topic expertise is unparalleled. We discuss the underlying process of atherosclerosis & the formation of plaques, ApoB, methods to stabilize plaque, metabolic syndrome and insulin resistance, markers and the risk of atherosclerosis, LP-PLA2 & atherosclerosis, homocysteine and cardiac risk, genetic therapies for lipid disorders. We also discuss lifestyle interventions, including exercise, in managing lipid disorders and reducing cardiovascular risk.
Dr. Dayspring Twitter:
https://x.com/Drlipid
Chapters:
01:07 Introduction
07:44 ApoB & Atherosclerosis
13:25 How Plaques Form
26:32 Stabilizing Plaque & Preventing Rupture
31:46 Metabolic Syndrome & Insulin Resistance
37:57 Markers & Risk of Atherosclerosis
40:42 LP-PLA2 & Atherosclerosis
47:00 Homocysteine & Cardiac Risk
57:14 Genet Therapies for Lipid Disorders
01:09:50 The Role of Exercise
Social & Website:
Instagram - / sterlingmdphd
Twitter - / sterlingmdphd
Facebook - / sterlingmdphd
TikTok - / sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F...
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
The content of this podcast is not medical advice, is for general information purposes only, and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. The content of this podcast is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
In this episode, I had the pleasure of sitting down with Nicolas Verhoeven of Physionic. We focus our attention on metabolic health and, specifically, the energy-related, cellular, and nutritional mechanisms of insulin resistance. Nicolas reviews evidence pertaining to the reversal of insulin resistance and dietary clinical trials demonstrating remission of type 2 diabetes. Nicolas also highlights the synergistic effects of physical activity and dietary habits on insulin resistance, expanding our discussion into mitochondrial health. Finally, we explore importance of a nuanced conversation around autophagy and its role in health and disease prevention.
Physionic on YouTube:
https://www.youtube.com/@Physionic
Chapters:
00:00:13 - Nicolas' Background & Inspiration
00:05:34 - Misconceptions about Carbs & Fat Intake
00:08:57 - Mechanisms of Insulin Resistance
00:18:34 - Reversing Insulin Resistance & Diabetes
00:23:08 - Measuring Insulin Resistance
00:24:20 - Continuous Glucose Monitoring (CGM)
00:30:25 - Insulin Resistance & Health
00:37:33 - Mitochondrial Dysfunction
00:49:14 - Mitochondrial Biogenesis
00:56:05 - Improving Mitochondrial Health
01:02:54 - Autophagy
01:07:28 - Closing Remarks
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F2sJXfnG63hSxJhT?si=40bb52e5b53f404c
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
The content of this podcast is not medical advice, is for general information purposes only, and does not constitute the practice of medicine or any other healthcare professional services. No doctor-patient relationship is formed. The content of this podcast is not a substitute for medical evaluation or treatment and does not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
In this episode, we discuss polarized training, which includes high-volume low intensity training and high-intensity training. We review the scientific literature pertaining to endurance performance, mechanisms of recovery debt, adaptations to various exercise modalities, and developing training programs around polarized training.
MAF-180: https://philmaffetone.com/180-formula/
#ultra #ironman #endurance #fitness #marathon
Chapters:
00:00 - Intro
01:20 - Athletic Burnout
02:36 - Endurance Training Distributions
03:37 - Recovery Debt
04:06 - Exercise-Induced Cardiac Fatigue
04:34 - Nervous System Fatigue
05:33 - Muscle Microtrauma
07:01 - Fitness Adaptations
08:56 - Maximum Aerobic Heart Rate
10:30 - Lactate Threshold
11:04 - High Intensity Exercise
11:57 - Polarized Training Program
13:05 - Outro
Social & Website:
Newsletter: http://eepurl.com/hQpdqT
Instagram: https://www.instagram.com/sterlingmdphd
Twitter: https://twitter.com/sterlingmdphd
Facebook: https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F2sJXfnG63hSxJhT?si=40bb52e5b53f404c
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
Does muscle loss occur in people taking GLP-1 receptor agonists such as semaglutide (marketed as "Ozempic" and "Wegovy") or combined GLP-1/GIP agonists like tirzepatide (marketed as "Mounjaro")? In this episode, we discuss current evidence regarding these next-generation weight loss drugs and muscle wasting, as well as principles of preventing muscle loss in weight loss programs.
#healthspan, #ozempic, #fitness, #muscle, #science
Chapters:
00:00 - Intro
00:30 - Importance of Muscle in Weight Loss
01:19 - Muscle Loss During Weight Loss
02:03 - What Affects Muscle Mass During Weight Loss?
02:16 - Clinical Trials
04:59 - Preserving Muscle During Weight Loss
05:30 - Protein Intake
06:28 - Strength Training
06:59 - Monitoring Body Composition
07:26 - Summary
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F2sJXfnG63hSxJhT?si=40bb52e5b53f404c
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
The content of this video is for general information purposes only and does not constitute the practice of medicine or any other healthcare professional services. The content of this video is not medical advice. No doctor-patient relationship is formed. The content of this video should not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
How do drugs like Ozempic (semaglutide) cause weight loss? In this episode, we discuss how these drugs (GLP-1 receptor agonists) target specific areas in the brain to suppress appetite and facilitate weight loss. We also discuss clinical trials data suggesting that these drugs and/or the weight loss that they facilitate may have cardioprotective effects. Lastly, we will also examine evidence regarding weight regain when coming off of these drugs and common side effects.
Link to episode on neuroscience of appetite regulation:
https://www.youtube.com/watch?v=i3RzV9vS_FA#healthspan, #semaglutide, #ozempic, #wegovy, #science, #weightloss
Chapters:
00:00 - Intro
01:31 - What Does GLP-1 Do?
02:08 - GLP-1 Receptors in the Brain
02:52 - Activating the GLP-1 "Switch" (Receptors)
04:13 - Clinical Trials - Semaglutide for Weight Loss
05:29 - Semaglutide and Heart & Metabolic Health
05:54 - For How Long Does Semaglutide Work?
06:35 - Weight Regain After Stopping Semaglutide
08:24 - Side Effects of GLP-1 Receptor Agonists
09:37 - Take-Home Points
10:20 - Outro
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F2sJXfnG63hSxJhT?si=40bb52e5b53f404c
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
The content of this video is for general information purposes only and does not constitute the practice of medicine or any other healthcare professional services. The content of this video is not medical advice. No doctor-patient relationship is formed. The content of this podcast should not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
Highly processed foods have been shown to lead to weight gain and are thought to drive intake through several mechanisms. Recent research suggests that the effect of combining fats and carbs on appetite might be more than the sum of their individual effects. Highly processed foods, accordingly, might simulate increased intake via the ratio of macronutrients.
Link to episode on neuroscience of appetite regulation:
https://www.youtube.com/watch?v=i3RzV9vS_FA
Study Link: https://doi.org/10.1016/j.cmet.2018.06.010
Errata: Hu et al. was published in 2018.
#diet, #weightloss, #science, #fitness, #food
Chapters:
00:00 Intro to Ultra-Processed Foods
00:51 Mouse Study on Macronutrients & Food Intake
01:34 Fat-to-Carb Ratio May Affect Food Intake
02:15 Brain Effects of Diet
03:26 Key Points
03:51 Study Limitations
04:23 Outro
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F2sJXfnG63hSxJhT?si=40bb52e5b53f404c
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
The content of this video is for general information purposes only and does not constitute the practice of medicine or any other healthcare professional services. The content of this video is not medical advice. No doctor-patient relationship is formed. The content of this podcast should not take precedence over information provided to you by your healthcare provider or official public health sources. Please visit nicksterling.com/terms for full Terms of Use.
Growing scientific evidence suggests that highly processed foods are associated with increased risk of disease. Until recently, scientists were unable to study directly the effects of highly processed foods on humans. In this episode, we review one of the first highly controlled scientific trials demonstrating that ultra-processed foods lead to weight gain.
Neuroscience of appetite regulation: https://youtu.be/i3RzV9vS_FA
#diet, #weightloss, #science, #fitness, #food
Chapters:
00:00 - Intro to Ultra-Processed Foods
00:55 - What are Ultra-Processed Foods?
02:14 - Disease & Ultra-Processed Foods
03:19 - Interventional Study
04:24 - Ultra-Processed Foods & Weight Gain
05:44 - Take-Home Points
06:57 - Outro
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F2sJXfnG63hSxJhT?si=40bb52e5b53f404c
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
In this episode, we discuss how overeating can lead to inflammation and neuron dysfunction in specific parts of the brain that control appetite and energy regulation. We review the neuroscience of appetite regulation, energy expenditure, and body fat regulation. Topics include hypothalamic dysfunction of body fat regulation, leptin resistance, neuro-inflammation, and physical changes in the hypothalamus involving microglia (the immune cells of the brain). We also review what is known about avoiding and reversing these changes.
Chapters:
00:00:00 - Introduction
00:00:37 - Brain Changes in Obesity
00:01:20 - Leptin Deficiency & Obesity
00:03:25 - Leptin Replacement
00:04:43 - Hypothalamic Obesity
00:05:42 - What is the Hypothalamus?
00:06:51 - Food Intake, Appetite, & VMH
00:08:50 - Ob Gene
00:09:34 - The Satiety Factor
00:11:11 - Leptin Paradox
00:11:51 - Leptin Resistance
00:13:41 - Leptin Physiology
00:15:03 - Leptin Resistance
00:18:11 - Effects of Leptin Resistance
00:18:29 - Improving Leptin Resistance
00:20:24 - Hypothalamic Inflammation
00:24:08 - Triggers of Hypothalamic Inflammation
00:25:45 - Fatty Acids & Hypothalamic Inflammation
00:26:24 - Advanced Glycation End Products (AGEs)
00:27:05 - Current Knowledge on Hypothalamic Inflammation
00:28:17 - Summary
00:30:16 - Outro
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://open.spotify.com/show/5TDUK3F2sJXfnG63hSxJhT?si=40bb52e5b53f404c
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
Is it possible to be metabolically healthy and overweight or obese? In this episode, we discuss the science of what makes fat healthy or unhealthy. We discuss how metabolic dysfunction in fat tissue can affect the rest of the body. We also review evidence pertaining to the "obesity paradox" and explore explanations for the associations of body mass index (BMI) and changes in the risk of disease complications and mortality. We discuss how metrics of central obesity can be used to obtain a better picture of an individual's metabolic health. Lastly, we discuss the critical link between exercise capacity and future health, as well as how to begin to transform our existing fat stores into a healthier state.
Chapters:
00:00 - Introduction
00:50 - Healthy Obesity as an Idea
02:36 - Concepts of Healthy vs. Unhealthy Fat
02:59 - Subcutaneous, Visceral, and Ectopic Fat
05:22 - Adipocyte Hypertrophy
06:36 - Fat Cell Insulin Resistance
08:19 - The Obesity Paradox
12:23 - BMI & Age
13:53 - Bariatric Surgery
15:51 - Limitations of BMI
16:26 - Lifetime Maximal BMI
16:37 - Metrics of Central Adiposity
18:30 - Metabolically Healthy Obesity
21:38 - Exercise & Metabolically Healthy Obesity
22:36 - Improving the Health of Fat
24:03 - Exercise Capacity & Risk of Death
25:29 - Zone 2 Training
26:51 - The Effects of Weight Loss (Fat Loss)
27:55 - Summary
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://spoti.fi/3mZDvMv
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
Maffetone Method:
https://philmaffetone.com/180-formula/
In this episode, we discuss fat through the lens of performance and survival, and what happens when we push our energy systems to their limits. We also talk about how our bodies make adaptations via exercise to improve our ability to "burn" fat for fuel, and how our bodies conserve fuel during times of negative energy balance. Lastly, we preview the role of fat as an endocrine organ and the importance of its communication with the brain, as well as the critical role of exercise capacity for our future health.
Chapters:
00:00 - Introduction
01:49 - Extreme Endurance
02:54 - Fuel Source & Effort
03:12 - Glycogen
05:16 - Using Fat for Fuel
08:48 - Known Limits of Prolonged Energy Expenditure
10:21 - Metabolic Rate & Endurance Duration
14:00 - Physiology of Fat
16:18 - Insulin & Catecholamines in Fat Metabolism
19:10 - Fat as an Endocrine Organ
21:05 - Exercise & Maximal Fat Oxidation
22:02 - Exercise & Future Health
22:55 - Summary
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://spoti.fi/3mZDvMv
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/
This is our first episode on weight gain and weight loss. In this episode, we describe how, as an industrialized nation, our food supply and environment have changed in a way that, in many cases, is mismatched with our biology as humans. We explore how these changes can lead to disease and metabolic dysfunction. We discuss how the replacement of whole foods with processed foods, as well as the addition of caloric sweeteners to most of the food items within grocery stores across the nation has preceded a rapid rise in obesity and metabolic dysfunction. In this episode, we begin to discuss some of the pathophysiology related to the consumption of ultra-processed and hyper-palatable foods as well as concerns surrounding the consumption of fructose- and glucose- containing sugary drinks. We also discussed the timelines of weight gain and loss as they typically occur over the lifespan and vary according to season. This episode sets the stage for the next episodes, which will focus on the normal fat metabolism and how it may become dysregulated in metabolic dysfunction.
Chapters:
00:00 - Introduction
01:21 - Metabolic health as a continuum
03:57 - Obesity as an epidemic
05:12 - Heritability and genetics of obesity
06:45 - Where obesity starts in the body
07:26 - History of weight gain in the U.S.
11:32 - High fructose corn syrup vs. table sugar
13:40 - Glycemic index and load
14:45 - What happens to your liver with sugary drinks
16:24 - Sugary drinks may be associated with cancerous changes
17:35 - The calories from sugary drinks are not automatically offset
20:24 - Obesity as a disease
23:10 - Obesity and kids
24:24 - How obesity develops across the lifespan
26:55 - The impacts of weight loss attempts
30:12 - Summary and upcoming content
Social & Website:
Instagram - https://www.instagram.com/sterlingmdphd
Twitter - https://twitter.com/sterlingmdphd
Facebook - https://www.facebook.com/sterlingmdphd
TikTok - https://www.tiktok.com/@sterlingmdphd
Newsletter - http://eepurl.com/hQpdqT
Subscribe to the Podcast:
Apple Podcasts: https://apple.co/3y438C9
Spotify: https://spoti.fi/3mZDvMv
Google Podcasts: https://bit.ly/3Olanei
References & Show Notes:
http://www.nicksterling.com/