Discover The secrets of alzheimer's disease
The secrets of alzheimer's disease

15 Episodes
Reverse
Alzheimer's disease (AD) represents a profound global health challenge, characterized by progressive neurodegeneration leading to severe cognitive decline and dementia. At its core, AD pathology involves the accumulation of toxic amyloid-beta (Aβ) species, particularly Aβ oligomers, and hyperphosphorylated tau protein aggregates within the brain. A persistent and formidable obstacle in the development of effective AD therapeutics has been the blood-brain barrier (BBB), a highly selective physiological interface that meticulously regulates the passage of substances into the central nervous system, often impeding the entry of promising therapeutic agents. Recent scientific advancements are fundamentally reshaping the approach to this long-standing challenge. Two distinct, yet complementary, strategies are demonstrating significant promise in preclinical and early clinical investigations: nanomicelle-mediated drug delivery and focused ultrasound (FUS) for temporary and targeted BBB modulation. These innovative methods are emerging as critical enablers, offering novel avenues to either deliver therapeutic compounds directly to the brain or to enhance the brain's intrinsic clearance mechanisms. Preclinical studies have shown that engineered nanomicelles can effectively encapsulate and deliver anti-Aβ oligomer antibody fragments across the BBB in mouse models, resulting in a significant reduction of toxic Aβ species and inhibition of plaque formation. Concurrently, early-stage human clinical trials involving focused ultrasound, even without the co-administration of drugs, have demonstrated safety, a reduction in amyloid plaques, and improvements in associated neuropsychiatric symptoms. While these groundbreaking developments are still in nascent stages and require further validation, they lay crucial groundwork for future combination therapies and represent a substantial leap forward in AD research, instilling renewed optimism in a field that has long grappled with limited therapeutic solutions.
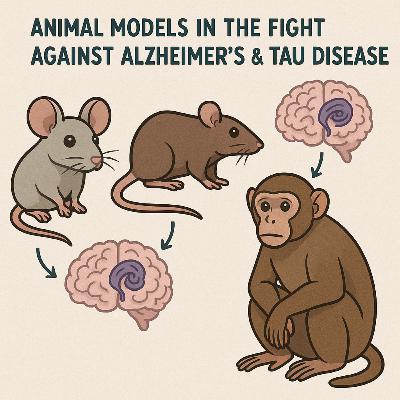
In vivo mouse models have been instrumental in advancing the understanding of tauopathies, a diverse group of neurodegenerative disorders characterized by the pathological accumulation of tau protein. These models, ranging from early transgenic lines to sophisticated humanized knock-ins and induced models, have provided critical insights into tau aggregation, prion-like spreading, synaptic dysfunction, neuroinflammation, and the complex interplay with amyloid-beta pathology. They serve as indispensable platforms for preclinical drug discovery, contributing to the development of therapies that modulate tau phosphorylation, aggregation, and clearance.Despite significant contributions, mouse models face inherent limitations in fully replicating the complexity of human tauopathies, including species-specific differences in tau biology, the challenge of dual amyloid-beta and tau pathology in Alzheimer's disease, and the incomplete recapitulation of post-translational modifications seen in late-stage human disease. These factors contribute to the persistent translational gap between preclinical success and clinical trial outcomes.However, the field is rapidly evolving. Emerging trends in advanced genetic engineering, particularly CRISPR/Cas9 technology, are enabling the creation of more precise, physiologically relevant models that avoid overexpression artifacts and allow for the study of specific tau isoforms and post-translational modifications. The integration of optogenetics and chemogenetics is facilitating circuit-specific mechanistic studies, while human induced pluripotent stem cell (iPSC)-derived organoids offer complementary human-specific in vitro platforms. Future directions emphasize the development of multi-factorial models that incorporate genetic and environmental risk factors, aiming to better mimic sporadic, age-related human tauopathies and ultimately enhance the predictive validity for therapeutic development.
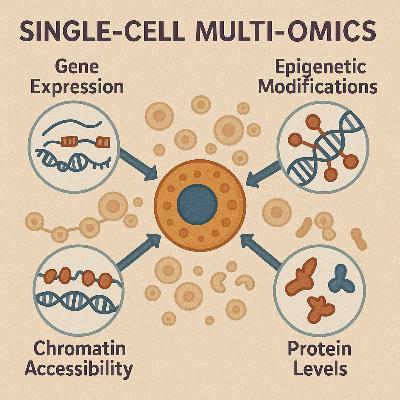
Next-Generation Sequencing (NGS) has fundamentally transformed biological research by enabling the rapid, high-throughput analysis of vast amounts of genetic material. This revolutionary technology allows for the simultaneous sequencing of millions of DNA or RNA fragments, dramatically reducing costs and accelerating scientific discovery compared to conventional methods. This report provides an in-depth examination of three pivotal NGS applications: poly(A) RNA sequencing (polyA RNA-seq), Assay for Transposase-Accessible Chromatin using sequencing (ATAC-seq), and single-cell RNA sequencing (scRNA-seq). PolyA RNA-seq offers a precise and quantitative view of the transcriptome, primarily focusing on messenger RNAs (mRNAs) and certain long non-coding RNAs (lncRNAs) to profile gene expression, identify novel transcripts, and analyze alternative splicing. ATAC-seq delves into the epigenome, mapping regions of open chromatin to reveal regulatory elements, transcription factor binding sites, and nucleosome positioning, thereby providing crucial insights into gene regulation. Complementing these bulk approaches, scRNA-seq provides unprecedented resolution by analyzing gene expression at the individual cell level, which is indispensable for dissecting cellular heterogeneity, identifying rare cell populations, and tracing developmental trajectories within complex biological samples. The combined application of these techniques in multi-omics approaches is generating a more holistic understanding of biological systems. By integrating insights from gene expression patterns and chromatin accessibility, researchers can delve deeper into complex processes, from cellular differentiation to disease progression, thereby driving the development of precision medicine strategies. Continuous advancements, particularly in spatial omics and long-read technologies, promise to further enhance the resolution and comprehensiveness of genomic and epigenomic profiling, enabling the study of molecular landscapes directly within their native tissue context.
Single-cell RNA sequencing (scRNA-seq) has fundamentally transformed our understanding of cellular biology by enabling the comprehensive profiling of gene expression at the resolution of individual cells. This contrasts sharply with traditional bulk RNA sequencing, which provides an averaged gene expression profile across a population, thereby obscuring the inherent heterogeneity within tissues and cell populations. ScRNA-seq unveils the vast array of RNAs within each cell, offering unprecedented insights into cellular diversity, the identification of rare cell populations, and subtle gene expression patterns that are otherwise masked by bulk measurements. The immense scale and complexity of scRNA-seq data, often encompassing thousands to hundreds of thousands of genes across tens of thousands to millions of cells, pose significant challenges for interpretation. In this high-dimensional landscape, effective data visualization becomes not merely an aesthetic choice but a critical analytical necessity. It empowers researchers to interactively process, interpret, and extract meaningful biological information, leveraging human cognitive abilities to discern visual structures such as clusters and outliers. Visualization serves as the essential bridge between raw data and biological discoveries, facilitating the identification of novel cell subtypes, the characterization of cell subpopulations, and the uncovering of underlying patterns and structures within complex biological systems. The computational ecosystem for scRNA-seq analysis is vast and continually expanding, with over 1,700 methods dedicated to single-cell RNA-seq alone. Navigating this extensive array of tools to produce reliable and cutting-edge results necessitates a deep understanding of the appropriate visualization techniques and the principles that underpin them. This report delves into the common plots employed in scRNA-seq analysis, detailing their purpose, the biological information they convey, their strengths, and their limitations, thereby providing a comprehensive guide for researchers.
single cell omic technology
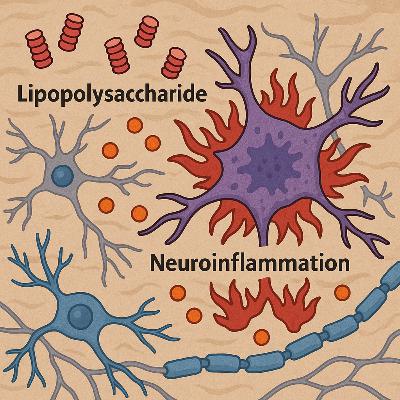
Neuroinflammation represents a pivotal pathological mechanism intricately linked to the onset and progression of a spectrum of neurodegenerative disorders, including Alzheimer's disease (AD), Parkinson's disease (PD), frontotemporal dementia, and amyotrophic lateral sclerosis. This inflammatory response within the central nervous system (CNS) is not merely a consequence of neuronal damage but actively contributes to the degenerative cascade. The Lipopolysaccharide (LPS)-induced animal model has emerged as a widely adopted and indispensable tool for investigating neuroinflammation, effectively replicating the behavioral dysfunctions and cellular pathological mechanisms observed in these complex conditions. The model's capacity to mimic systemic inflammation, which is known to exert detrimental effects on the nervous system and cognitive functions, underscores its relevance in preclinical research. The widespread adoption and continued significance of LPS models in neuroinflammation research are fundamentally driven by the increasingly established causal link between chronic inflammatory processes and the pathogenesis of neurodegenerative disorders. By experimentally inducing this inflammatory component with LPS, researchers can directly probe the mechanisms underlying disease development and rigorously evaluate potential therapeutic interventions. This capability positions the LPS model as a crucial bridge for understanding the intricate relationship between inflammation and neurodegeneration.cc
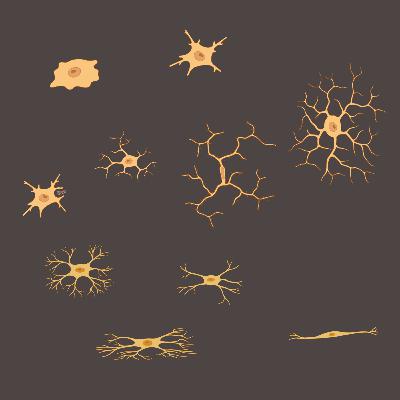
Despite the remarkable progress in elucidating the roles of microglia and astrocytes in AD, the exploration of oligodendrocytes, another major glial cell type, in the context of this neurodegenerative disorder remains in its nascent stages. Their involvement has been largely underappreciated and understudied, particularly when compared to their glial counterparts. Some researchers suggest that oligodendrocytes might represent a crucial, previously unidentified element in our comprehension of AD and related dementias. While traditionally recognized for their primary function in the production of myelin, the insulating sheath around nerve fibers, their other potential roles within the context of neurodegeneration have only recently begun to be extensively investigated. Contrary to the long-held notion of oligodendrocytes as passive bystanders in the development and progression of AD pathology, emerging evidence strongly indicates their active participation in and reaction to both amyloid and tau pathology, the two primary hallmarks of the disease. This paradigm shift suggests that oligodendrocytes are not merely affected by the AD environment but actively contribute to its pathogenesis and progression. Recent research employing advanced techniques such as RNA sequencing and single-cell analysis has revealed that oligodendrocytes express genes and proteins associated with AD pathology, hinting at a more direct role in the disease than previously conceived. This report aims to review the recent advancements in understanding the multifaceted roles of oligodendrocytes and their myelin sheaths in the context of AD, thereby shedding light on their complex interactions within the intricate framework of the disease pathology.
The potential roles of a new type modification on RNA in AD context.
An m6A reader moderates the neuroinflammatory response through translation regulation.
Alzheimer's disease (AD) stands as a prevalent and debilitating neurodegenerative disorder, primarily affecting the aging population. It is characterized by a progressive decline in cognitive function, prominently manifesting as memory loss, ultimately leading to dementia. The neuropathological hallmarks of AD include the extracellular accumulation of amyloid-beta (Aβ) plaques and the intracellular formation of neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau protein. Despite extensive research efforts, current therapeutic interventions for AD remain limited, primarily offering symptomatic relief without effectively halting or reversing the underlying disease progression. This limitation underscores the urgent need for the development of novel therapeutic strategies that target the fundamental mechanisms driving AD. Increasingly, the scientific community recognizes glial cells, particularly astrocytes, as crucial players in the initiation and progression of AD pathology. While the amyloid cascade hypothesis, focusing on Aβ and tau, has long dominated AD research, the limited success of treatments targeting these pathologies has prompted a broader investigation into the roles of other cellular components within the brain. The growing body of evidence implicating astrocytes in various aspects of AD pathogenesis positions them as promising targets for future research and the development of more effective therapeutic interventions.
Recent research has further illuminated the concept of "stressed" microglia and their altered functions in driving neurodegeneration. Activation of a cellular stress pathway known as the integrated stress response (ISR) within microglia has been found to prompt these cells to produce and release toxic lipids. These lipids can then damage neurons and oligodendrocyte progenitor cells, which are crucial for maintaining brain function and are significantly affected in Alzheimer's Disease. This discovery suggests that cellular stress can fundamentally alter the behavior of microglia, leading to neurotoxic outcomes that contribute to the progression of AD.
Alzheimer's disease (AD) represents a significant and growing global health challenge, characterized by progressive cognitive decline and neurodegeneration. While the accumulation of amyloid-beta (Aβ) plaques and neurofibrillary tangles of tau protein have long been considered the primary pathological hallmarks of AD, an increasing body of evidence highlights the critical role of neuroinflammation in the disease's onset and progression. Recent approvals of Aβ-targeting therapies like lecanemab and donanemab underscore the importance of pathways regulating Aβ accumulation, where neuroinflammation plays a significant part. These advancements indirectly emphasize the interconnectedness of amyloid pathology and neuroinflammatory processes in AD. Furthermore, the emergence of novel neuroinflammatory biomarkers offers promising avenues for earlier diagnosis and more effective monitoring of disease progression. Consequently, a substantial amount of ongoing research and numerous clinical trials are now focused on directly targeting neuroinflammation as a therapeutic strategy for AD. Despite the considerable progress in understanding the role of neuroinflammation, translating these insights into effective treatments presents several challenges, and future research will be crucial in overcoming these hurdles to develop meaningful therapies.
Neurodegenerative diseases represent a growing global health crisis, characterized by the progressive dysfunction and loss of neurons in the central nervous system.1 Among the pathological hallmarks of these debilitating conditions, the accumulation of neurofibrillary tangles (NFTs) composed of the microtubule-associated protein tau stands out as a critical factor in a diverse group of disorders known as tauopathies.1 Alzheimer's disease (AD), the most prevalent neurodegenerative disease, is also the most common tauopathy, where the extent and distribution of tau accumulation in the form of NFTs exhibit a strong positive correlation with the severity of cognitive impairment and dementia.1 Beyond AD, a spectrum of other tauopathies, including Pick's disease (PiD), progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), and various forms of frontotemporal dementia (FTD), are defined by the presence of abnormal tau inclusions.1 The sheer diversity of diseases associated with tau aggregates underscores the fundamental importance of deciphering the intricacies of tau pathology to pave the way for effective therapeutic interventions.The strong correlation between tau pathology and cognitive decline has spurred intense research efforts aimed at developing therapeutic interventions that specifically target tau protein and its aggregation into neurofibrillary tangles.3 Several promising therapeutic avenues are currently being explored, each with a unique mechanism of action.
The amyloid cascade hypothesis proposes a specific sequence of pathological events initiated by the abnormal accumulation of amyloid-beta in the brain. The cascade is thought to begin with the aberrant processing of the amyloid precursor protein (APP), leading to either an overproduction or a decreased clearance of Aβ peptides, particularly the Aβ42 isoform. These Aβ peptides then undergo a process of aggregation, initially forming small, soluble oligomers. These oligomers are increasingly recognized as the primary toxic species in the cascade. Subsequently, these oligomers are believed to aggregate further, forming insoluble amyloid fibrils that eventually deposit in the extracellular space as amyloid plaques. According to the hypothesis, the presence and accumulation of these amyloid plaques, and particularly the more toxic soluble oligomers, then trigger a series of downstream pathological events within the brain. These events are thought to include the hyperphosphorylation of tau protein, leading to the formation of neurofibrillary tangles within neurons, the activation of glial cells resulting in chronic neuroinflammation, the disruption of synaptic function and loss of synapses, and ultimately, neuronal death. This cascade of pathological changes is proposed to be the underlying cause of the progressive cognitive decline and memory loss that are characteristic of Alzheimer's disease. The amyloid cascade hypothesis, therefore, provides a framework for understanding the temporal sequence of pathological events in AD, although the precise mechanisms and the relative importance of different Aβ forms, particularly the transition from plaques to oligomers as the main culprit, are areas of ongoing refinement and investigation.
Alzheimer's disease (AD) represents a significant global health challenge as the most prevalent cause of progressive neurodegenerative disorder and dementia. The intricate pathology of AD is characterized by several key features within the brain, most notably the accumulation of amyloid plaques, the formation of neurofibrillary tangles, and chronic inflammation.