Discover Greater Sydney Area HEMS
Greater Sydney Area HEMS

19 Episodes
Reverse
G'day, and thanks for tuning in to another episode of the HEMS Debrief podcast - this is our focused series on cardiac arrest.
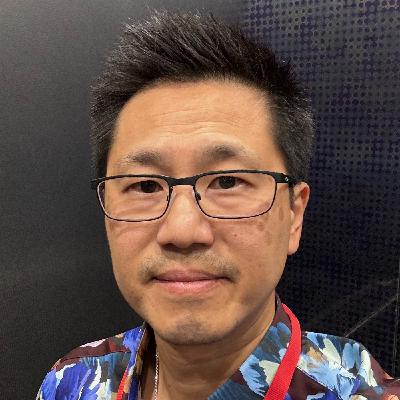
Today we are joined by Canadian Physician-Researcher Dr Brian Grunau. Brian is an Assistant Professor at the University of British Columbia Department of Emergency Medicine and works clinically as an Emergency Physician at St. Paul’s Hospital in Vancouver, Canada. His research investigates methods to improve outcomes from out-of-hospital cardiac arrest, and in so doing he has received over $15 million in research funding and published over 190 peer-reviewed articles. Brian is a member of the International Liaison Committee on Resuscitation (ILCOR) Advanced Life Support Task Force, which creates resuscitation treatment recommendations.
In today's episode, we specifically quiz Brian on the time dependent yields of conventional resuscitation vs eCPR initiation, as well as how a system can best promote cardiac arrest research at every step of the chain of survival.
Thanks as ever for listening!
As we move deeper into 2026, the podcast will re-introduce episodes on more general Retrieval / Aeromedical topics, addressing both the technical and non-technical of this fascinating and challenging speciality. Do hit subscribe to stay up to date! And as ever, thank you for listening.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
G'day and welcome back to the HEMS debrief podcast.
It is 2026, and we are kicking off with an episode of the cardiac arrest mini-series dedicated to paediatric cardiac arrest.
Sadly Nat could not join, so instead Sam alone is in conversation with Dr Janice Tijssen.
Janice is a paediatric critical care physician from London, Ontario. Having trained in London (Ontario) and Toronto, Janice is now a member of the Paediatric Life Support Taskforce for the International Liaison Committee on Resuscitation (ILCOR) and is the medical director for her hospital's Paediatric Advanced Life Support (PALS) education program. Too, Janice leads her hospital's Paediatric Critical Care Outreach Team (PCCOT).
In this episode, we reflect on the changes in the recent ILCOR guidelines around paediatric cardiac arrest, as well as deep dive into some of the physiology of the arrested paediatric patient, asking both how can we prevent arrest, and how can we optimise the arrested physiology to best achieve sustained ROSC.
We sure hope you enjoy this episode, there is a lot in here for any paediatric critical care provider.
As we move deeper into 2026, the podcast will re-introduce episodes on more general Retrieval / Aeromedical topics, addressing both the technical and non-technical of this fascinating and challenging speciality. Do hit subscribe to stay up to date! And as ever, thank you for listening.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
G'Day and welcome back to the HEMS debrief, cardiac arrest mini-series. This is part two of our conversation with the pre-hospital ECMO team from Paris, France.
Following part one, in this part two we continue to chat with Alice and Lionel about their extended research in the out-of-hospital cardiac arrest space, including but not limited to rapid cooling and ventilation strategies.
Too, we discuss the cultural reluctance of systems to further adopt pre-hospital ECMO, as well as share some tips for those systems considering embarking on ECMO provision.
As 2025 draws to a close, thank you sincerely for listening throughout 2025, and we cannot wait to talk again in 2026.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
G'day and welcome back to the Sydney HEMS Debrief podcast - this is our focused mini-series on Cardiac Arrest.
Today's episode is a big one. We have the absolute privilege of speaking to the Dr Alice Hutin and Prof Lionel Lamhaut from the pre-hospital ECMO team in Paris, France.
The team, part of the Service d’Aide Medical d’Urgence (aka SAMU) in Paris, have been performing pre-hospital ECMO for OOHCA since 2011. For the past 10 years, the team have been available 24/7, working in concert with the pre-hospital ICU team dispatched to cardiac arrests in the greater Paris region.
Truly ground-breaking, Alice and Lionel join us to reflect on over a decade of pre-hospital ECPR care, system implementation and challenges. Too, and perhaps most significantly, Alice and Lionel reflect on the extent to which the pre-hospital ECPR service has influenced every step of the chain of survival in the Paris system - promoting high quality basic and advanced life support at multiple levels within the pre-hospital response.
Too, Sam does not shy away from asking some tough questions around just who should be performing ECPR - high specialised, limited access services or should this therapy be adopted and delivered more widely.
This is part one of a two part episode, and is an absolute cracker.
Be sure to tune in to part two very soon!
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
G'day and welcome back to the Sydney HEMS debrief, with our focus still firmly on cardiac arrest.
In this episode 14, Nat is joined by Dr Helen Oliver in conversation with Dr Caroline Leech from the UK. Caroline is an emergency and pre-hospital physician who's academic interest focuses on maternal cardiac arrest. Specifically, Caroline's work concerns resuscitative hysterotomy; the when, the how, and the what to do after performing this HALO procedure.
Additionally, Nat, Helen and Caroline discuss the physiology of maternal cardiac arrest and how we can best optimise our holistic resuscitation care as well as some of the ethical considerations surrounding this very challenging and confronting circumstance.
We hope you enjoy this challenging episode, and of course share widely with your network.
Chat soon.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Welcome back, this is part two of Nat's chat with Dr PO Berve from Norway.
Continuing the conversation, Nat and PO discuss physiological markers of ALS effectiveness as well as broach how to most judiciously use adrenaline during cardiac arrest. Too, PO dives into how to use the end tidal capnogram as a marker of CPR effectiveness - and it is not how you may think!
Of course, this would not be a Sydney HEMS debrief episode without talking about eCPR and ventilation during CPR - the later being a favourite topic of Nat's for sure.
As ever, thanks for listening and chat again soon.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
As we move our the podcast onto both Spotify and Apple Podcasts, we are re-posting this episode originally published in March 2024.
In this episode, Nat and Alex join Sam to discuss the Sydney PRECARE pre-hospital ECMO trial as it is just getting under way. Focusing on workflows and team integration, Nat and Alex share their experiences, challenges and successes in these early days for the trial.
We hope that the content here may help frame that of other episodes in this cardiac arrest series, as well as flavour future episodes as we reflect on PRECARE several years later.
Hello, and welcome back to the Sydney HEMS debrief podcast. This is our focused series on cardiac arrest.
Today we have part one of two in conversation with Dr PO Berve from Norway. PO is an Anaesthetist and Pre-Hospital physician from Oslo where he works on the physician response car of the region. PO's research has been absolutely fundamental to the modern understanding of CPR physiology and the haemodynamics of the arrested patient, and his work is rightly lauded as critical in the practice of physiology-guided resuscitation.
Have you ever wondered what happens during one chest compression? In this episode, Nat deep-dives with PO into the physiology of the arrested patient – specifically what happens, or what should happen, during one perfect chest compression. It’s a fascinating conversation not to be missed by anyone with an interest in performing high quality resuscitation tailored to a specific patient.
Part two coming soon!
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Welcome back to the Sydney HEMS debrief. We are up to episode 11!
Today, we are pivoting towards toxicology. Specifically, we discuss some of the more common toxidromes encountered pre-hospitally, how they cause cardiac arrest, and what providers – in particular pre-hospital providers – may do in order to best resuscitate these patients.
In addition to some broader and very applicable learning themes pertinent to any toxidrome, we discuss
Beta-blockers
Calcium channel blockers
Amitriptyline
Quetiapine
…and more
Of course we are not doing discussing this alone. We are so luck to be joined today by a clinical toxicologist, Dr Úna.
Dr Úna Nic Ionmhain graduated from Trinity College Dublin, and subsequently trained in Emergency Medicine in Perth. She completed a Pre Hospital and Retrieval Medicine year with CareFlight NSW as well as a poisons fellowship. She is now a staff specialist FACEM at Liverpool Hospital NSW, and a clinical toxicologist with the NSW Poisons Information Centre. She has an academic interest in HIET in toxicology for cardiogenic shock, which was the focus of her masters thesis, and is a passionate educator with a particular interest in cardiotoxicity.
We sure hope you enjoy this episode, and until next time, we hope you have a great week.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
This is part two of our conversation with Dr Mike Lauria.
Join us as Nat and Mike continue to delve into team performance. In this episode, Nat and Mike discuss human factors gold including but not limited to how to accept imperfection and continue to deliver optimal team performance when things are going south, how to instil calm in a team whilst maintaining the momentum of care, and how to adapt and pivot whilst maintaining optimal process.
Of course, there is much much more and so we hope you enjoy this episode, and share it far and wide.
Speak soon.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello, and welcome back to the Sydney HEMS debrief podcast.
Thank you for your patience – I have been taking the long way home from Canada, but am delighted to be back in Sydney and now ready to go with more episodes of our focused series on cardiac arrest.
In this part one of two episodes, we are pivoting away from the technical towards human factors and team performance. In doing this, we are thrilled to be joined by Dr Mike Lauria.
Mike is a human factors legend. Prior to becoming a Doctor, Mike served as an elite Pararescueman in the 321st Special Tactics Squadron during which time he won numerous service awards. Then, Mike became the lead instructor of a tactical training group before moving back to New Hampshire to work as a Critical Care and Flight paramedic. If that wasn’t enough, Mike then went to and graduated from Medical School before completing his residency in Emergency Medicine, as well as fellowships in EMS and Critical Care, at the University of New Mexico Health Science Center.
Currently, Mike works as an attending critical care and EMS physician at the University of Washington, and is the Associate Medical Director at Airlift Northwest.
Suffice to say, Mike brings an exceptional wealth of experience and perspective on what constitutes a high performing team and a high performing individual, and the factors required to maintain operational momentum even during unfavourable circumstances. Nat and Mike discuss this and much more in what are two episodes full of absolute gold.
I predict these episodes will become mandatory listening for human factors and team performance enthusiasts, and rightly so.
Chat soon!
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello and welcome back to the Sydney HEMS debrief, focus on cardiac arrest.
This week, we are very excited to deep dive into defibrillation. Join us as we talk through the physics of defibrillation, what is needed to get defibrillation as good as it can be, and what to do when defibrillation is simply not working.
We are delighted to be joined this week by Michael Heller. Michael is a paramedic by background, who now works as a medical engineer focused on defibrillation. Michael studied Rescue Engineering in Germany, and combining his clinical background is now a defining expert voice on defibrillation, and an excellent educator.
Too, we are delighted to be joined again by CCP Jackie, the educator for the Sydney pre-hospital ECMO/cardiac arrest car. In this episode, Jackie reflects on her experience backing up crews attending cardiac arrests, and how this experience has shaped her appreciation of the importance of good and judicious defibrillation, the barriers to making this happen, and how we as providers can all improve our defibrillation practice.
We hope you enjoy this episode, and as ever please send any feedback to me (Sam).
Have a great week!
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello and welcome back to the Sydney HEMS debrief, focus on cardiac arrest.
This week, we are joined by a Sydney local – Prof Jimmy Chien, as we talk about PE in cardiac arrest.
Jimmy is a Senior Staff Specialist (Senior Consultant) in Respiratory Medicine, with a sub-speciality focus on pulmonary embolism. Jimmy has been fundamental in the creation of the PE emergency response team at his tertiary facility in Sydney, as well as in the roll-out of similar multi-disciplinary teams across Australia. On a daily basis, Jimmy and his team encounter the most challenging PE patients – those with intermediate or high risk PE, as well as those in arrest.
In this episode, Nat, Jimmy and I unpack how a PE causes an arrest, how to ascertain if a patient has arrested secondary to a massive PE, the therapies available to those patients who have arrested due to a known or suspected PE, and the role of mechanical support including ECMO. Too, we quiz Jimmy on where the literature is taking us to help manage this cohort of patients, as well as some of the emerging post-therapy care plans.
Jimmy is a wealth of knowledge, and we sure hope you enjoy the episode as much as we did recording it.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello and welcome back.
This week, we are joined by Dr Felipe Teran from New York, discussing trans-oesophageal ECHO (TOE) in arrest.
Felipe is an Associate Professor of Emergency Medicine at Weill Cornell Medical College, New York. Additionally, Felipe is a clinical scientist and educational leader specifically focused on the utility and application of TOE during cardiac arrest. Indeed, Felipe is leading the way integrating this intervention into ACLS efforts.
In this episode, myself (Sam), Nat and CCP Jackie chat with Felipe about the literature to date demonstrating the application of TOE in arrest to best optimise chest compression position to promote forward flow. In so doing, resuscitation providers can attempt to avoid a left ventricular outflow tract obstruction, and are better able to continually assess the effectiveness of ACLS – noting that the heart can change position throughout arrest.
Additionally, Nat talks about her and the team’s experience of pre-hospital TOE within the New South Wales Ambulance system, in particular how TOE can be utilised as part of a toolkit of assessment during arrest to assess the effectiveness of a resuscitation – even in the absence of placing a patient onto ECMO. Linked to this, Jackie describes the effect of live physiologic guidance and feedback to the paramedic workforce in New South Wales.
We certainly hope you enjoy this episode, and we look forward to talking with you again soon.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello and welcome back.
As we continue to discuss cardiac arrest, this week we talk with Prof Laurie Morrison from Toronto about:
How to integrate cardiac arrest research into an existing systems
How to gather and interpret physiologic data during arrest – particularly ventilation data – and what to do with this data to optimise arrest care
How to be a leader in this research field
Prof Morrison is an academic and Clinical Scientist in the Division of Emergency Medicine, Department of Medicine at the University of Toronto and Sunnybrook Health Sciences Centre. Her program of research focuses on the evaluation and implementation of time sensitive interventions in acute emergencies, including cardiac arrest.
Laurie is a member of ILCOR, where she has been named a ‘Giant in Resuscitation’. Outside of ILCOR, Laurie has led the way establishing ‘Rescu’ – a collaborative prehospital research network wherein investigators conduct randomised controlled trials and outcome validation studies in resuscitation research. Laurie continues to provide leadership to several committees including the network of Canadian Emergency Medicine Researchers, and she has has received honorary membership to the European Resuscitation Council for life time achievement in resuscitation science.
We hope you enjoy this episode, and as ever please send us feedback or questions.
Please remember to hit subscribe!
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello, and welcome back to the Sydney HEMS debrief, focus on cardiac arrest.
This is the second half of our chat with Dr Hans van Schuppen from Amsterdam as we put the P back into CPR.
In today’s episode, we discuss amongst other things:
Lung recruitment intra-arrest
The impact of tidal volumes during arrest
To PEEP or not to PEEP during arrest
How to use ventilation to prevent acidosis during arrest
Join now as we continue to pick Hans’ brain, and as ever we hope you enjoy this and subsequent episodes.
Please remember to hit subscribe!
Here is a link to the text Hans’ references concerning common terminology of ventilation during cardiopulmonary resuscitation: https://pubmed.ncbi.nlm.nih.gov/39848430/
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello, and welcome back to the Sydney HEMS debrief, focus on cardiac arrest.
This is episode 3, and today it is all about ventilation during arrest. It is time to put the P back into CPR. Ventilation has been neglected in cardiac arrest management, and this two part episode focuses on how ventilation can not only help achieve a ROSC but the importance of ventilation too in achieving neurologically intact survival
We debate 30:2 or continuous ventilation and the merits of LMA vs intubation vs BVM
We talk about the complexities of heart lung interactions
Where the research is heading in understanding how best to ventilate these patients
We are delighted to be joined by an absolute expert in this area, Dr Hans van Schuppen from Holland.
Hans is an anesthesiologist and HEMS physician at the Amsterdam University Medical Centre. Hans is a combined researcher, clinician and leader. He is an ERC Advanced Life Support Course Director, co-founder of the ResusNL conference, member of the expert group on national ambulance guidelines on resuscitation and is a member of the jury of the Dutch National Resuscitation Competition. As a member of the Dutch Resuscitation Council, he co-authored the national resuscitation guidelines, and helped to develop and implement a nationwide standard operating procedure for the handover of out-of-hospital cardiac arrest patients.
Currently, Hans is the chair of the Medical Committee and board member of the Dutch Resuscitation Council. His research evolved into a formal PhD with the ARREST (AmsteRdam REsuscitation STudies) group and the department of Anesthesiology, resulting in his thesis “Prehospital Advanced Life Support”. He now serves as director of resuscitation science of ARREST and works towards close collaboration between clinical care, education, research and innovation in resuscitation.
We could not stop talking to Hans, so please tune back in next week for the second half of our conversation.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello, and welcome back to the Sydney HEMS debrief, focus on cardiac arrest.
In the second episode of this series, we talk to Dr Tommaso Scquizatto from Milan, Italy.
Tommaso is a Doctor, researcher and innovator in cardiac arrest, resuscitation, and emergency critical care medicine. He works in the Department of Anaesthesia and Intensive Care at IRCCS Ospedale San Raffaele in Milan, Italy, where he leads cardiac arrest research and innovation.
His clinical and research efforts focus on improving the entire chain of survival for out-of-hospital cardiac arrest, from prevention to advanced resuscitation, including the use of extracorporeal life support and novel technologies. He serves on the Advanced Life Support (ALS) Task Force of the International Liaison Committee on Resuscitation (ILCOR) and the 2025 Guidelines Working Groups for BLS, ALS, and extracorporeal CPR of the European Resuscitation Council (ERC). He is also an editorial board member and social media editor for Resuscitation and Resuscitation Plus.
With Tommaso in this episode, we talk about targeted physiology in cardiac arrest included targeted diastolic blood pressure, Tommaso’s research, and how systems and workflows may adapt to incorporate new intra-ACLS interventions such as transoesophageal ECHO.
We hope you enjoy the episode, please be sure to hit subscribe and tune back in next week.
We are delighted to be sponsored by Corpuls - delivering high-tech and innovative equipment for emergency and intensive care medicine for over 35 years.
Hello, and welcome back to the Sydney HEMS debrief, focus on cardiac arrest.
This is the first in a series of podcasts dedicated entirely to cardiac arrest, the physiology driving the clinical presentation and how we can more effectively use physiological principles and basic science to underpin clinical care and research.
In this week's episode, we have the privilege of talking with Dr Paul Rees.
Who better to talk all things myocardial perfusion and it’s optimisation during cardiac arrest than an interventional cardiologist and pre-hospital physician. Paul explains the physiology of cardiac arrest from an interventional cardiologist perspective as we ask him the hard questions on:
Optimal diastolic blood pressure thresholds to improve ROSC
The role of adrenaline in improving coronary artery perfusion, the downside to it’s administration and the potential alternatives
The role of selective aortic aortic arch perfusion (SAAP), the current ERICA study and the potential for this procedure to improve cardiac arrest survival
The key elements in building a successful endovascular resuscitation program for those services wishing to embark on ECPR and/or REBOA
We hope you enjoy this episode, please contact Sam or Nat if you have any comments or questi