Discover The Healthcare Policy Podcast ® Produced by David Introcaso
The Healthcare Policy Podcast ® Produced by David Introcaso

The Healthcare Policy Podcast ® Produced by David Introcaso
Author: David Introcaso, Ph.D.
Subscribed: 41Played: 203Subscribe
Share
© David Introcaso, Ph.D.
Description
Podcast interviews with health policy experts on timely subjects.
The Healthcare Policy Podcast website features audio interviews with healthcare policy experts on timely topics.
An online public forum routinely presenting expert healthcare policy analysis and comment is lacking. While other healthcare policy website programming exists, these typically present vested interest viewpoints or do not combine informed policy analysis with political insight or acumen. Since healthcare policy issues are typically complex, clear, reasoned, dispassionate discussion is required. These podcasts will attempt to fill this void.
Among other topics this podcast will address:
Implementation of the Affordable Care Act
Other federal Medicare and state Medicaid health care issues
Federal health care regulatory oversight, moreover CMS and the FDA
Healthcare research
Private sector healthcare delivery reforms including access, reimbursement and quality issues
Public health issues including the social determinants of health
Listeners are welcomed to share their program comments and suggest programming ideas.
Comments made by the interviewees are strictly their own and do not represent those of their affiliated organization/s.
www.thehealthcarepolicypodcast.com
The Healthcare Policy Podcast website features audio interviews with healthcare policy experts on timely topics.
An online public forum routinely presenting expert healthcare policy analysis and comment is lacking. While other healthcare policy website programming exists, these typically present vested interest viewpoints or do not combine informed policy analysis with political insight or acumen. Since healthcare policy issues are typically complex, clear, reasoned, dispassionate discussion is required. These podcasts will attempt to fill this void.
Among other topics this podcast will address:
Implementation of the Affordable Care Act
Other federal Medicare and state Medicaid health care issues
Federal health care regulatory oversight, moreover CMS and the FDA
Healthcare research
Private sector healthcare delivery reforms including access, reimbursement and quality issues
Public health issues including the social determinants of health
Listeners are welcomed to share their program comments and suggest programming ideas.
Comments made by the interviewees are strictly their own and do not represent those of their affiliated organization/s.
www.thehealthcarepolicypodcast.com
327 Episodes
Reverse
At least one in four girls suffers childhood sexual abuse. For example, the Department of Justice (DoJ) concluded Jeffery Epstein trafficked over 1,000 girls, some as young as 14. Nevertheless, six years after Epstein’s reported suicide, the Trump Administration’s 2026 budget proposes to entirely delete a subsection of federal law that requires DoJ’s Office of Violence Against Women to be “a separate and distinct office” and proposes to cut the Office of Violence Against Women’s budget by nearly 30%. Per the CDC’s Adverse Childhood Experiences (ACEs) study, launched over 25 yrs ago, at least 1 in 4 girls and 1 in 20 boys are sexually abused. Among numerous other sobering stats, ACEs-related health consequences cost the US an estimated $14.1 trillion dollars annually in direct medical spending and lost healthy-life years. Dr. Frank Putnam, a child and adolescent psychiatrist at the U. of North Carolina’s Medical School who has spent his 35-year professional life investigating the effects of childhood sexual abuse on child development and adult outcomes, has recently completed “Old Before their Time” an autobiographical account of his research work and findings. In Dr. van der Klok’s introduction to the book, he states childhood sexual abuse “embeds itself in a child’s mind, body and behavior and is expressed across generations.” Deterrence “is the most powerful target for the prevention of mental illness and for reducing premature death from common illnesses.”Information regarding “Old Before Their Time” is at: https://www.amazon.com/Old-Before-Their-Time-Investigating/dp/1032974826. Dr. Frank Putman’s bio is at: https://www.med.unc.edu/psych/people/frank-w-putnam-md/. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
The US has effectively always suffered a physician shortage. Last year the AMA estimated a shortage of 86,000 by 2035. US policymakers have since 1965 addressed this problem by recruiting foreign born physicians (termed Foreign Medical Graduates or FMGs), mostly from Southeast Asia, largely India. Today FMEs, that account for 25-30% of the physician workforce, are disproportionately employed in Health Professional Shortage Areas or HPSAs in which there remains or persists a strong demand, e.g., HRSA recognizes over 7,500 primary care HPSAs. Nevertheless, Prof. Alam concludes stratifying our medical system can be interpreted in part as a cover up to a problem of long-term disinvestment in rural healthcare and minority health. Simply growing the work force has had, Prof Alam argues, both a minimal impact on the equitable distribution of US healthcare resources while intensifying global health inequalities resulting from substantial brain drain.Information about Prof. Alam’s book is at: https://www.press.jhu.edu/books/title/53838/care-foreigners?srsltid=AfmBOopgVAOX_1s9S7NaIMoKsXgrUS2htC4_HaE0zTYDrfQJltnIpRK7. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Over roughly the past year Prof. Blumberg and her Georgetown Center for Health Insurance Reform (CHIR) colleagues have been researching healthcare providers and payers increasing use of third-party entities they collectively termed “middlemen” with whom providers and payers contract to provide various supportive administrative or financial services. For example, payers frequently use of Third Party Administrators/TPAs and providers of Revenue Cycle Managers/RCMs. The use of middlemen is a problem because these entities are “rent seeking,” meaning they profit without creating new or additional value, thereby reducing economic efficiency and competition and driving prices up. In CHIR’s October report titled, The Complex Web of HC Fin Interests & Their Implication for Even Higher Spending,” Prof. Blumberg and her colleagues concluded relationships with middlemen have “resulted in a complex web of cost increasing incentives, money flows, and conflicts of interest. The complexity is so tremendous that it is virtually impossible to capture the entire picture of the existing financial relationships.” (Listeners may recall interviewed Leigh’s Prof. Katz-Olson in March 2022 regarding her related work, “Ethically Challenged, PE Storms US Health Care.” CHIR writings discussed during this interview include:https://chir.georgetown.edu/events/why-health-care-costs-are-rising-the-role-of-corporatization-and-bipartisan-solutions-to-increase-affordability/https://chir.georgetown.edu/events/why-health-care-costs-are-rising-the-role-of-corporatization-and-bipartisan-solutions-to-increase-affordability/https://chir.georgetown.edu/evidence-on-private-equity-suggests-that-containing-costs-and-improving-outcomes-may-go-hand-in-hand/https://chir.georgetown.edu/third-party-administrators-the-middlemen-of-self-funded-health-insurance/https://chir.georgetown.edu/independent-dispute-resolution-process-2024-data-high-volume-more-provider-wins/CHIR’s publication page is at: https://chir.georgetown.edu/search/?filter=publications This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Even though PC is the only component of healthcare shown to increase life expectancy and is crucial to achieving healthcare equity, outcomes, quality and value PC remains on life support. For example, an August National Academy of Medicine report concluded, “despite PC’s essential value for the health of the nation, more than 100 million people across rural and urban communities in the US are experiencing a calamitous lack of access to primary care.” Among numerous problems: PC accounts for less than 5% of total healthcare spending; there are too few primary care clinicians and too many, at 7,501, HRSA PC shortage areas; PC clinicians are inadequately reimbursed and maldistributed. Consequently, PC struggles to adequately address prevention, the social determinants of health, integrate care particularly behavioral health services and ultimately achieve optimal value. In “Wonderful and Broken,” Prof. Brennan discusses how PC care can be improved and organizations that are at least on the path toward stable and effective PC delivery. (Listeners may recall I interviewed Prof. Brennan in October 2024 regarding his just published previous work, “The Transformation of American Health Insurance” & that this is at least my 5th PC discussion dating back to 2013.)Information on Prof Brennan’s book is found at: https://www.press.jhu.edu/books/title/54051/wonderful-and-broken?srsltid=AfmBOor4SJMCBvCYWck_6Aobdxk-ZUJgusnceOxxT-eghoU8CkPc3kMl. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Because healthcare today can be increasingly defined as commodified, expedient, financialized, myopic, reductionist and failing to transcend politics, the question of healthcare’s ethics or the roll ethics plays should play is increasingly begged. For example, last October Health Affairs launched an “Ethics and Health Systems Change” series that to date has simply complained about private equity and corporate medicine, federal immigration and gender care policies and de-professionalization. What fidelity does healthcare have to normative ethics when, for example, 27 million Americans and counting are uninsured, over 100 million lack a primary care provider and over 90 million cannot afford care if they needed today. Dr. Jain, President and CEO of the SCAN Group and SCAN Health Plan, discusses the causes of healthcare’s ethical erosion and how begged ethical issues or questions can be addressed. The two Forbes articles authored by Dr Jain and discussed during this interview are at: https://www.forbes.com/sites/sachinjain/2025/09/22/ethical-erosion-how-good-people-lose-their-way-in-healthcare/ and https://www.forbes.com/sites/sachinjain/2025/01/21/who-me-ethical-erosion-and-the-deafening-silence-of-americas-healthcare-leaders/. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
This past summer CMS, more specifically CMMI, announced a six-year Medicare Part A demonstration that would require hospitals in six states to submit claims for prior authorization (PA) approval by non-medical, CMS-contracted, 3rd party entities using enhanced technologies, i.e., AI, for 17 medical items and services. Private/commercial Medicare or Part C Medicare Advantage plans have for years extensively used PAs though data suggests Medicare Advantage PA use has been excessive, e.g., a very high percentage of PA denials are reversed upon appeal) and widely viewed as a tool to enhance profit taking. CMMI-contracted tech/AI companies will be compensated based on a share the money saved from PAs contractors’ deny though subject to meeting quality criteria. The WISeR demo has attached a fair amount of criticism, e.g., 12 Senate Democrats and 17 House Democrats each wrote letters to HHS/CMMI noting their concerns that include the demo will present patient roadblocks, cause some patients to abandon care, risk denying necessary care, inflict substantial administrative burden on clinicians, perversely incent AI contractors and they argued Americans do not want AI involved in their healthcare decisions. The July 1 Federal Register WISeR notice is at: https://www.govinfo.gov/content/pkg/FR-2025-07-01/pdf/2025-12195.pdf.The CMS/CMMI WISeR website is at: https://www.cms.gov/priorities/innovation/innovation-models/wiser.Liu and Wadhera’s NEJM Perspective essay re: the WISeR demo is at: https://www.nejm.org/doi/abs/10.1056/NEJMp2510451. Don Berwick and Andrea Ducas’s STAT opinion essay re: the WISeR demo is at: https://www.statnews.com/2025/07/25/medicare-advantage-prior-authorization-cms-innovation-center-wiser-project/. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
The World Health Organization (WHO) defines patient safety as “a framework of organized activities to reduce risks, lower the occurrence of avoidable harm, make errors less likely, and minimize their impact when they occur.” Over this past summer the HHS Office of the Inspector General (OIG) published three patient-safety reports. (Since 2008 the OIG has published at least 24 related studies.) One published in July found hospitals failed to capture half of harm events that occurred among hospitalized Medicare patients, few were investigated and even fewer led to hospitals making PS improvements. These findings were sadly unsurprising since the OIG previously found in 2008 that 27% of Medicare patients experienced harm during hospital stays, a decade later, or in 2018, still 25% experienced harm. In an July 24 OIG letter to CMS Administrator, Dr. Mehmet Oz, the OIG noted in part that while CMS and states require hospitals to publicly report just 15 of 94 harm events, hospitals reported only 5 of 15, or 5% of all 94 harm events. HHS has yet to publicly respond to the OIG’s recent reports much less recognize them. Dedicated podcast listeners may recall I’ve previously discussed patient safety in 2015, 2017 and in 2020.A summary of the HHS OIG’s adverse events/patient safety work with a list of its publications can be found at: https://oig.hhs.gov/reports/featured/adverse-events/. Information regarding Mr. Millenson is at: https://millenson.com/.Mr. Millenson’s recent medical errors essay in Forbes is at: https://www.forbes.com/sites/michaelmillenson/2025/09/12/lessons-from-the-medical-error-that-orphaned-a-cabinet-secretary/. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Recently published research by Prof. Wrigley-Field and her colleagues found that between 1980 and 2023 the total number of US excess deaths equaled 14.7 million. Between 2010 and 2023 excess deaths ranged between 120% and 130% higher compared to other HIC (High Income Countries). Possibly more disturbing the authors found US excess deaths were moreover among working-age adults, for example, in 2023 excess deaths among US adults aged 25-44 were 2.6 times higher than in other HIC. That same year excess deaths remarkably made up almost 23% of all deaths and 46% of excess deaths were among people younger than 65 years. The causes of excess deaths since 1980 have on balance largely been the result of preventable cardiometabolic causes and drug overdoses. About these findings, Prof Wrigley-Field’s coauthor, Prof. Jacob Bor, commented, “if the US simply performed at the average of our peers, one out of every two US deaths under 65 years is likely avoidable. Our failure to address this is a national scandal.” Prof. Wrigley-Fields writings discussed during this podcast are at: https://jamanetwork.com/journals/jama-health-forum/fullarticle/2834281https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2829783https://www.annualreviews.org/content/journals/10.1146/annurev-soc-031021-105213 This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
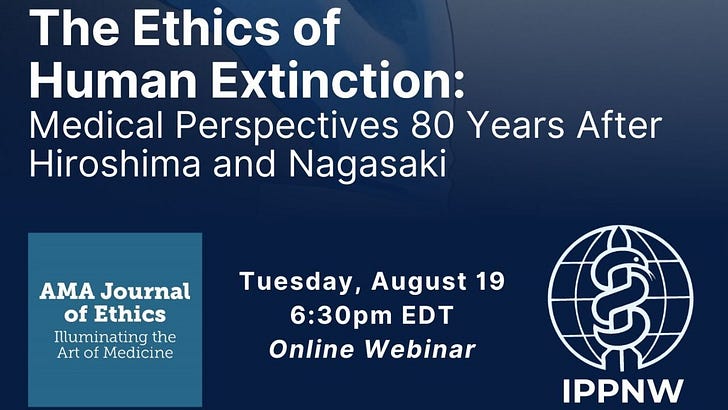
The greatest threat to human health is us. Humans are the only species capable of self-annihilation. For at least the past 30 years it has been acknowledged that the earth is presently experiencing its sixth mass extinction entirely caused by anthropogenic GHG emissions. Per research published in 2023, current generic extinction rates are 35 times higher than expected background rates prevailing in the last million years under the absence of human impacts. Research published in Proceedings, the National Academy of Sciences (PNAS) in 2022 concluded, “There is ample evidence that climate change could be catastrophic. We could enter such “endgames” at even modest levels of warming.” “Facing a future of accelerating climate change while blind to worst-case scenarios is naïve risk management at best and fatally foolish at worst.”Mr. Kellis’s August article (and related podcast), “Why Should Extinction Medicine Be a Specialty?” appears in the recent AMA Journal of Ethics special issue on extinction medicine, at: https://journalofethics.ama-assn.org/issue/existential-health-care-ethicsThe recent SSRN pre-print on extinction medicine is at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5109482The recent IPPNW-AMA Journal of Ethics webinar on the ethics of human extinctions: To sign up for the Extinction Medicine Reading Group, a new IPPNW Medical Student Movement initiative that will promote international, intergenerational, and interdisciplinary discussion on writings on the science, ethics, and medicalization of human extinction, go to: https://forms.gle/pLspc5URhu9VcuS37Mr. Kellis can be reached via : www.devinkellis.com This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
On July 23rd the United Nations’ International Court of Justice (ICJ) announced its highly-anticipated climate advisory opinion. The opinion represents a watershed moment because the court ruled states or countries are accountable for contributing to anthropogenic warming or for their GHG emissions. Consequently, the ICJ concluded countries are legally obligated to ensure the climate is protected from GHG emission, if not, countries - and private actors such as healthcare - can be held culpable for failing to do so. Though an advisory opinion the ICJ ruling has significant implications for US healthcare largely because US healthcare annually accounts for a massive amount of GHG emissions at over 600 MMT of CO2e and the federal government has neither enacted legislation nor promulgated regulations that require healthcare mitigate its GHG emissions. Not surprisingly, healthcare has ignored the 2023 UN resolution that requested the ICJ opinion and now the opinion. The ICJ opinion is at: https://www.icj-cij.org/case/187/advisory-opinionsThe Columbia University Sabin Center’s Climate Change Law Blog ICJ symposium writings are at: https://blogs.law.columbia.edu/climatechange/category/blog-series/ This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
The climate crisis is not a tragedy. It’s a crime. The July 4 signing of HR1, is the latest if not the greatest climate crime considering the current state of the earth’s energy imbalance or the ever-increasing amount of atmospheric GHG emissions that trap infrared radiation (heat) causing planetary warming. It’s estimated the OBBBA will over just the next five years add an extra seven billion tons of GHG emissions into the atmosphere - equal to more than one-years’ worth of total annual US carbon emissions. While it had been projected the US would reduce GHG emissions this decade by upwards of 43%, or get close us to a 50-52% reduction to align with the 2015 Paris Accord, the OBBBA will now reduce carbon emissions this decade by just 17%. The legislation rescinds virtually all IRA renewable energy tax credits while further subsidizing fossil fuels. Prof. Jacobson’s considerable contribution to understanding and addressing climate breakdown can be found at: https://web.stanford.edu/group/efmh/jacobson/. Information regarding his most recent book, “No Miracles Needed” (U. of Cambridge Press, 2023), is at: https://web.stanford.edu/group/efmh/jacobson/WWSNoMN/NoMiracles.html. Prof. Jacobson’s LinkeIn page is at: https://www.linkedin.com/in/mark-jacobson-1b58b38/. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Last week’s signing of the OBBBA serves as federal policymakers’ latest reverse Robin Hood effort, or to redistribute wealth from the poor to the rich. Per a February RAND report, over the past 50 years $79 trillion in wealth has been redistributed from the bottom 90% of Americans to the top 1%. The 2017 Trump tax cult left billionaires $6 trillion richer and the OBBBA, otherwise termed the Bill for Billionaires Act, is expected to achieve similar of not greater results largely because the number of billionaires has dramatically increased to nearly 2,000 over the past decade. The legislation is (partially) offset moreover by cutting Medicaid spending by upwards of $1 trillion that is expected to lower Medicaid enrollment by 11 million and cause 17,000 premature deaths annually. SNAP spending will be reduced $300 billion leaving three million even more hungry. The bill will add an estimated 3.8 trillion to the deficit, atop the $8.4 trillion left by the first Trump administration. Financing the deficit that approximates $1 trillion annually represents more than the DoD’s budget or money that could be spent on other things - like healthcare. Largely because of increasingly regressive tax policies and unaffordable healthcare, studies conclude the bottom 60% of US households by income are unable to achieve what is s defined as a "minimal quality of life" or one in which families can afford adequate housing, healthcare, child care and food. See these two related research efforts by Prof. Ferguson, “Political Investments” at: https://www.phenomenalworld.org/interviews/thomas-ferguson/ and Ferguson, et al., “How Much Can the US Congress Resist Political Money?” at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3593916. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Anthropocentric warming, the greatest threat to human health and survival, disproportionately threatens children. Children pay the greatest climate penalty. Per the World Health Organization, children suffer more than 80% of climate crisis-related injuries, illnesses & deaths being more vulnerable to carbon-polluted air, extreme heat, drought and innumerable other climate-charged disasters and diseases. Nevertheless, the US healthcare accounts for an ever-increasing amount of carbon pollution and refuses to divest in fossil fuels. As for federal policymakers, the White House and Congressional Republicans remain intent on committing ecocide. To the surprise of no one, in late May Our Children’s Trust, on behalf of 22 plaintiffs age 7 to 25, sued President Trump and five administrative offices and departments arguing in part several White House Executive Orders will increase fossil fuel use and dismantle climate research, warnings and response infrastructure. The lead plaintiff in Lighthiser v Trump stated White House policy amounts to a “death sentence for my generation.” The WCC handbook available at: https://www.oikoumene.org/news/wcc-publishes-resource-on-legal-tools-for-climate-justice. The Lighthiser v Trump complaint is at: https://climatecasechart.com/case/lighthiser-v-trump/.Among related discussions, I interviewed the Michael Burger at Columbia University’s Sabin Center for Climate Change Law in May 2020 and again in June 2024 and Andrea Rodgers with Our Children’s Trust this past January. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Frequent listeners of this podcast are well aware healthcare emits an immense amount of carbon pollution at over 600 million metric tons annually. This is substantially due to energy waste or inefficiency. For example, hospitals, that account roughly 35% of the industry’s GHG emissions, loses or forgoes tens billions in annual revenue or explicit and implicit lost opportunity costs. Healthcare pays in several ways for its energy inefficiency. Among other reasons, though one of the world’s most high tech sectors, healthcare still largely consumes electricity produced by burning fossil fuels. Heat-generated electricity is significantly less efficient than use of renewable energy technology that avoids converting heat to electricity or work. Renewable energy is increasingly more price efficient (that explains why 92% of new electricity produced in 2024 was via renewables). Healthcare utilization or demand is increased as a result of healthcare’s carbon pollution and hospitals already face market headwinds, moreover the fact inflation-adjusted payment rates have been stagnant to negative for several years. Information on Eneration can be found at: https://www.eneration.com This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Due to the federal government’s ongoing failure to effectively address the climate crisis, over 50 subnational entities have been taking increasingly aggressive steps to mitigate carbon pollution. Recently, Vermont (VT) and New York (NY) passed legislation to hold the oil and gas industry financial responsible for extreme weather events supercharged by their greenhouse gas (GHG) emissions. (Eleven other states are presently working to do the same.) The VT law tallies up the financial damage and then determines proportional responsibility; NY identifies in advance a damage amount and then proportionally bills responsible fossil fuel companies. VT and NY’s legislation is based attribution science. Simply explained, the methodology attempts to measure to what extent anthropocentric warming caused by fossil fuel use of specific entities supercharges extreme weather events. Last month, Stanford’s Dr. Christopher Callahan and Dartmouth’s Dr. Justin Makin published, “Carbon Majors and the Scientific Case for Climate Liability in the journal “Nature.” The authors calculated the trillions of dollars in economic losses attributable to the extreme heat caused by emissions from individual companies or carbon majors. For example, emissions attributable to Chevron caused between $791 billion and $3.6 trillion in heat-related losses between 1991 and 2020. Drs. Callahan and Mankin’s April 24 “Nature” article is at: https://www.nature.com/articles/s41586-025-08751-3 (subscription is required).A summary of the article is freely available via “The Guardian,” at: https://www.theguardian.com/environment/2025/may/05/cost-of-emissions-from-five-major-australian-resource-companies-more-than-900bn-study-finds. Info on Dr. Callahan is at: https://profiles.stanford.edu/326897 and for Dr. Mankin, at: https://geography.dartmouth.edu/people/justin-s-mankin. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Despite the fact US healthcare has $7.6 trillion market cap and is beyond capital intensive, industry executives have been loathe to divest in fossil fuels. For example, per “The Lancet’s” 2023 and 2024 annual “Countdown on Health and Climate” reports, between 2008 and 2023 of the 1,613 institutions committed to divesting in fossil fuels, only 28 were healthcare institutions and since 2018 only one has committed to doing so. Among numerous other reasons why this is, to be polite, disturbing, if not evil, is because: fossil fuel investments substantially explain healthcare’s massive carbon footprint at over 600 MMT of CO2e annually; anthropocentric warming poses the greatest threat to human health; failure to divest make a mockery of the Hippocratic Oath; and, among other ironies of the 12 S&P 500 economic sectors the energy sector was the worst performer by far since 2010. Information regarding the First Do No Harm campaign, including their sign-on letter, is at: https://firstdonoharm.earth/. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
US healthcare costs and spending are extreme made evident by the fact healthcare at a $5 trillion annually accounts for roughly half the global healthcare market. This reality led Princeton’s Nobel Prize Economist Angus Deaton to conclude in 2020, “the industry is a cancer at the heart of the economy.” Though healthcare costs are projected to rise 7 to 8%, this year, cost growth over the past 15 plus years plus has not on average exceeded GDP growth - made evident by the fact that while the 2020 Medicare Trustee report concluded the Medicare hospital trust fund would be bankrupt by 2026, the most recent report concluded 2036. Prof. Buntin’s recent writing on the topic, “The Value Zeitgeist, Considering the Slowdown in Healthcare Spending Growth,” coauthored by Harvard’s Ellen Meara and Dartmouth’s Carrie Colla, was published in “The New England Journal of Medicine” on April 12th. Prof Buntin’s recent publications are at: https://hbhi.jhu.edu/expert/melinda-buntin. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
At present, measles, one of the most contagious communicable diseases for which there is no treatment, disproportionately sickens - and kills - preschoolers. The outbreak is present today in 21 states ranging from Alaska to Vermont. As of last Friday, this year has already seen 607 confirmed cases, 72% of cases were among those age 5 to 19 and 97% of those infected were either unvaccinated or their vaccination status is unknown. For comparison, for five-year period ending in 2024 the average number of annual measles cases equaled 105.The measles, mumps, and rubella (MMR) vaccine is exceptionally effective and when immunization is greater than 95%, herd immunity is achieved. Having previously attained this percent measles was considered officially eliminated in the US in 2000. Achieving measles elimination was considered an historic public health achievement. Today however approximately 40 of states have vaccination rates below 95%. As a result, public health officials, for example in West Texas, expect the outbreak to continue for the remainder of this year, if not beyond.Concerning the federal government’s response this past Sunday when asked about the outbreak , President Trump stated, “It’s so far a fairly small number of people relative to what we’re talking about,” adding, “this is not something new.” Beyond cutting CDC staff and state funding to monitor infection/disease transmission, the White House is withdrawing the US from the World Health Organization (WHO) that in part managed a networks of labs, entirely funded by the US, to track measles cases around the world. HHS Secretary Robert Kennedy, a man with an anti-vaccination history, recently stated the measles vaccine is the “most effective way to prevent the spread” of the disease, however, he continues to frame vaccination as a personal choice and suggest the vaccine can cause just as much harm as the disease itself. Hours after making his “most effective” comment, the Secretary highlighted the work of doctors treating infected children with steroids and an antibiotic. The Secretary has also noted cod liver oil and Vitamin A as treatments. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
The Trump administration has made no secret it intends to aggressively enforce immigration laws, made evident by the recent arrest of a Columbia University grad student and green card holder on Columbia’s campus. Since the White House has repeatedly stated it intends to deport roughly all 12 million undocumented immigrants, this presents an immediate problem for healthcare providers who, in part, have legal and ethical obligations to all their patients. This is particularly true ironically for HHS-regulated Federal Qualified Health Centers (FQHCs) who serve 32 million largely racial/ethnic minorities who, because they are largely poor and medically disenfranchised, are disproportionately in need of healthcare. One day after assuming office in January the acting Department of Homeland Security rescinded decades of prior policy that essentially stated the federal government would not take immigration enforcement action in “protected areas” that included healthcare facilities - and schools like Columbia University. Ms. Smith’s most recent writing on the topic, “ICE in your Healthcare Facility? No Need to Freeze,” is at: https://www.dorseyhealthlaw.com/ice-in-your-healthcare-facility-no-need-to-freeze/. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com
Two weeks after being sworn in, last Friday HHS Secretary Robert Kennedy announced, “effectively immediately, the [1971] Richardson Waiver is rescinded and is no longer policy of the Department.” He explained his decision by stating “the extra-statutory obligations of the Richardson Waiver impose costs on the Department and the public, are contrary to the efficient operation of the Department, and impede the Department’s flexibility to adapt quickly to legal and policy mandates. “ The waiver, issued by President Nixon’s HEW Secretary, Elliot Richardson, effectively meant HHS would use the 1946 Administrative Procedure Act’s “notice of proposed rule making” (NPRM) process broadly and its “good cause” exception sparingly. (The APA essentially governs the process by which federal agencies develop and issue regulatory rules.) Secretary Kennedy rescinded the waiver citing APA language that exempts rule making, effectively public input, from matters “relating to agency management or personnel or to public policy, loans, grants, benefits or contracts” and permits departments to forgo public comment for “good cause” or when the procedure is “impracticable, unnecessary or contrary to the public interest.” Though Secretary Kennedy’s decision will almost certainly be challenged in court, in the near term HHS can make significant, and now unquestioned, regulatory changes to, for example, the Medicare and Medicaid programs. Sec. Kennedy’s one page, March 3 Federal Register notice is at: https://www.govinfo.gov/content/pkg/FR-2025-03-03/pdf/2025-03300.pdf. This is a public episode. If you would like to discuss this with other subscribers or get access to bonus episodes, visit www.thehealthcarepolicypodcast.com