232: How your pelvic health affects your lifestyle and sexual health: navigating perimenopause, menopause and more with Marie-Josée Forget
Description
In this episode, we welcome Marie-Josée Forget. Marie-Josée is a bilingual Pelvic Health Physiotherapist, educator, and mentor with 18 years of clinical experience. She operates a private physiotherapy practice focused on treating pelvic floor dysfunction and teaches courses related to pelvic anatomy and health at Pelvic Health Solutions. Marie-Josée Forget speaks with us about women's health. We learn about perimenopausal, and menopausal women and their pelvic health. How your pelvic health affects your lifestyle and sexual health, Kegel exercises, navigating perimenopause, menopause, and more!
SPONSOR
BETTERHELP
BetterHelp is the largest online counseling platform worldwide. They change the way people get help with facing life's challenges by providing convenient, discreet, and affordable access to a licensed therapist. BetterHelp makes professional counseling available anytime, anywhere, through a computer, tablet or smartphone.
Sign up today: http://betterhelp.com/solvinghealthcare and use discount code “solvinghealthcare"
Thank you for reading Solving Healthcare Media with Dr. Kwadwo Kyeremanteng. This post is public so feel free to share it.
Solving Healthcare Media with Dr. Kwadwo Kyeremanteng is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
TRANSCRIPT
KK: We are on the brink of a mental health crisis, and this is why I am so appreciative of the folks over at BetterHelp. It provides the largest online counseling platform worldwide to change the way people get help with facing life's challenges by providing convenient, discreet, and affordable access to licensed therapists. BetterHelp makes professional counseling available anytime, anywhere through a computer, tablet, or smartphone. Sign up today. Go to betterhelp.com And use a promo code ‘solvinghealthcare’ and get 10% off signup fees.
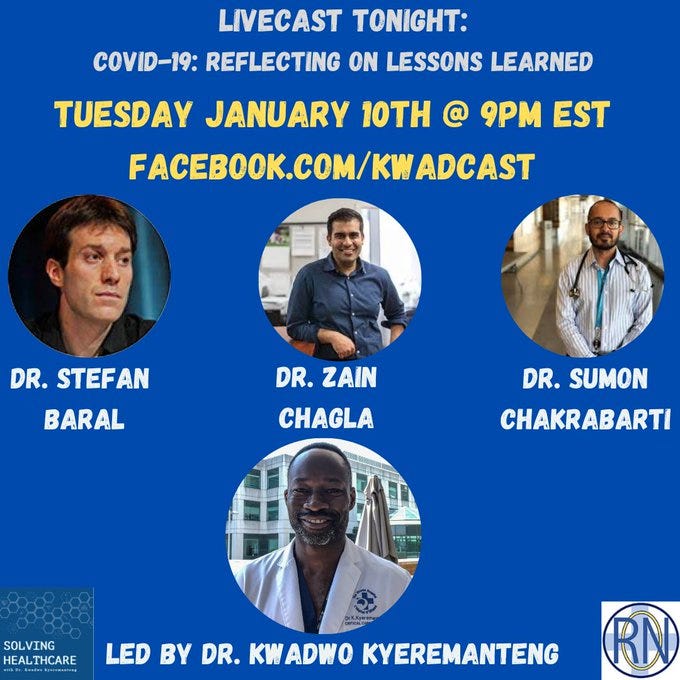
SP: COVID has affected us all and with all the negativity surrounding it, it's often hard to find the positive. One of the blessings that is given us is the opportunity to build an avenue for creating change. Starting right here in our community discussing topics that affect us most such as racism and health care, maintaining a positive mindset, creating change, the importance of advocacy, and the many lessons we have all learned from COVID. If you or your organization are interested in speaking engagements, send a message to kwadcast@gmail.com, reach out on Facebook at Kwadcast or online at drkwadwo.ca
KK: Welcome solving healthcare. I'm Kwadwo Kyeremanteng. I'm an ICU and palliative care physician here in Ottawa and the founder of ‘Resource Optimization Network’ We are on a mission to transform healthcare in Canada. I'm going to talk with physicians, nurses, administrators, patients and their families because inefficiencies, overwork and overcrowding affects us all. I believe it's time for a better health care system that's more cost effective, dignified, and just for everyone involved.
KK: Kwadcast nation welcome back. We have a tremendous episode with MJ Forget. She is a pelvic floor specialist in physiotherapy and sees a lot of perimenopausal women and was really knowledgeable in terms of the issues that she sees firsthand. Many people can benefit from a pelvic floor physio, for example, if they're having incontinence, pain or with sexual health, this is such an important aspect of things. Then she dives into how holistic the approach must be how the physio can actually make some significant strides. How lifestyle changes can impact things. Honestly, I learned so much in this episode. So, we'll jump on it right away here. But first, I want to give a quick plug to our latest newsletter on substack kwadcast.substack.com. Where you can stay up to date with all our releases, our blogs, or blogs or guest appearances, courses all are on one site and it's all point. Check out kwadcast.substack.com and jump on the train. So, without further ado MJ Forget.
KK: Welcome to the show. We we've been talking more about women's health, specifically, perimenopausal and menopausal women. One of the areas that I must say it was a bit foreign to me and I didn't realize it was such a big issue was pelvic health. So MJ you've been at this for a while, like when you started? You said over 20 Maybe 25 years?
MJ: 25 years? Yeah.
KK: What lured you to pelvic health and like how big of an issue has is pelvic health ben for people?
MJ: When we graduate from university, you know, and the medical fields we get to find areas of interest when we graduate and that's kind of all that we do. And you know physio, some of them want to do orthopedics and work with sports teams. When I graduated, I went to the hospital system, which is a lot of what physios do, and I worked in ICU and I worked on the floors, I did orthopedics, post knee posts, hips, and it really wasn't where my passion lied by any means. But it was a really great introduction to all thing’s physios working in a hospital setting. So, when I thought about where do I want to go? And what do I want to do? I always had an interest at the time what we call more women's health. Now we call it pelvic health because again, all genders have pelvic health issues. I had classmates who did their thesis on incontinence. I remember thinking at the time oh my gosh “That's something that we can do?”. It really wasn't anything we were taught in university, nobody really talked about, again pelvic health, women's health, women's health issues, menopause, that was never covered in our degree. So, I took my first course and Alberta back in 1997 and I never looked back. I had no idea how much pelvic health issues was a problem. Remember 25 years ago, nobody talked about any of that. Nobody talked about bladder control issues or bowel control issues. Certainly, nobody talked about menopause, and nobody talked about sexual health, which is a lot of what we do in pelvic health. So, I started my career, like I said, I was in my early 20s and that's all I've been doing now, for 25 years. This is where I'm at.
KK: Wow. You alluded to, you didn't realize how big of a problem it was, like how big of a problem truly is it?
MJ: If we talk just about incontinence in Canada, if we just talk about general stats in Canada, 3.3 million Canadians have bladder issues in Canada. When we think about gender differences, one in four women, one of one to nine men, so it's significant. It actually gets a little worse as we age. That's an issue with menopause. So, if we think about the female population, there's about a 20% to 30% incidence of incontinence in our young adulthood. Think of like your 20s and 30s. Then that spikes up to almost 40%. By the time we get into middle age, which is kind of the perimenopausal menopausal age. Then it goes up as high as 50% in our elderly, which is a really big concern. One of the main reasons that our clients get admitted into nursing homes is because of bladder issues, and fecal incontinence rate, loss of bladder and bowel control is usually kind of an event where families then have a hard time maybe coping with taking care of their of their loved ones, and that will increase admissions to nursing homes. So, we're not talking about small numbers. It's a significant number and we have an aging population in Canada. We have a lot of people going through perimenopause and menopause. One of the biggest risk factors of incontinence is actually menopause. We have a lot of people right now who are entering kind of that phase, you know, and I think in Canada, the stats are that there's 10 million of us in this age group in perimenopause, heading into menopause in Canada. That's a big number.
KK: It's massive. And I think this is what's motivated us to cover some of this content because these are years of productivity, have high needs, like moms that are in that perimenopausal age where you're active with your family, your career paths, like a lot of people this is where they're starting to peak in their careers, a lot of demands just to be to be on the workforce, like when I think of health care workers. So, anything we could do to make them more functional and thrive. I think we need to really look at. I don't know if I realized that, like this is kind of like the peak or one of the main concerns during the perimenopausal perimenopausal menopausal timeline. What can you do? What do you do to help?
MJ: There's so much we can talk about this for hours, but we'll try to kind of keep in to keep our timeline because I can get started. I mean, if we're just going to focus on, we’ll talk the impact of perimenopause and menopause. Like you said, it's such a difficult time. You know, people going through perimenopause and menopause, like you said, are working. They are often parents, with children that still require a lot of our attention. Plus, sometimes we're taking care of our parents as well. We're kind of like in that middle group where we're busy with our careers. We may or may not have children, but we also may have parents that we help and it's a really stressful time, and quality of life really starts to take an impact. So typically, when people come to see a pelvic health physiotherapist, or a physiotherapist who's done postgraduate studies in pelvic health, what we do is we are often seeing people that come for problems of bladder control and bowel control. So that would say that's kind of when I started that was the most of what I've seen, but we also help our patients with sexual function and the ability to have pain free sexual intercourse, which is a big issue again in perimenopause and it can actually worsen and menopause as well. We help with conditions called pelvic pain, pelvic