ASH 2025 Orlando: Childhood Leukemia Cured But Families Broke! “Financial Toxicity” is Often More Worrying than your Child’s Cancer
Description
ASH 2025 Orlando: Childhood Leukemia Cured But Families Broke. “Financial Toxicity” is Often More Worrying than you Child’s Cancer
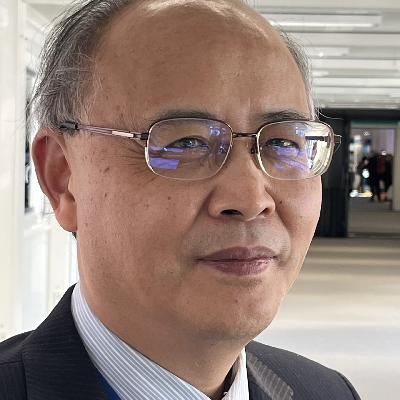
An interview with: Daniel Zheng, Instructor, Children’s Hospital of Philadelphia, Attending Oncologist, Division of Oncology, Philadelphia PA, United States
ORLANDO, USA—Although most children with acute lymphoblastic leukemia can look forward to a cure, their families may face catastrophic financial hardship, according to Daniel Zheng, an Instructor and Attending Oncologist at the Division of Oncology, Children’s Hospital of Philadelphia in Philadelphia, PA, United States. After reporting on the challenge families face of “financial toxicity” from extended curative treatment for ALL Dr. Zheng talked about his findings from the Dana Farber Cancer Institute ALL 16-001 Trial with Audio Journal of Oncology correspondent, Peter Goodwin:
Audio Journal of Oncology: Daniel Zheng
IN: “[GOODWIN] I’m reporting direct … OUT: Oncology, I’m Peter Goodwin 7:38 secs
American Society of Hematology 2025 Annual Meeting Abstract 710:
“Cumulative incidence of household material hardship and income loss as measures of financial toxicity during pediatric acute lymphoblastic leukemia (ALL) treatment: A report from the DFCI: ALL 16-001 Trial”
Authors
Daniel Zheng1, Eva Robinson 2, Yael Flamand, 3, Rahela Aziz-Bose 4, Victoria Koch3, Peter Cole5, Lisa Gennarini6, Kelly Getz7, Justine Kahn8, Kristine Karvonen9, Colleen Kelly10, Kara Kelly11, Bruno Michon12, Haley Newman1, Morgan Paul13, Thai Tran14, Puja Umaretiya15, Jennifer Welch16, Edie Weller2, 17, Lewis Silverman8, Kira Bona 10
1 Children’s Hospital of Philadelphia, Division of Oncology, Philadelphia, PA, United States,
2 Boston Children’s Hospital, Biostatistics and Research Design Center, Boston, MA, United States,
3 Dana-Farber Cancer Institute, Boston, MA, United States,
4 Dana-Farber Cancer Institute, Department of Pediatric Oncology, MD, MPH, MA, United States,
5 Rutgers Cancer Institute, New Brunswick, NJ, United States,
6 Montefiore Medical Center, Bronx, NY, United States, 7 University of Pennsylvania, Department of Epidemiology, Philadelphia, PA, United States, 8 Columbia University Irving Medical Center, Division of Pediatric Hematology, Oncology and Stem Cell Transplantation, New York, NY, United States,
9 Seattle Children’s Hospital, Division of Pediatric Hematology-Oncology, Seattle, WA, United States,
10 DanaFarber Cancer Institute, Department of Pediatric Oncology, Boston, MA, United States,
11 Roswell Park Comprehensive Cancer Center, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, Department of Pediatrics, Buffalo, NY, United States,
12 Centre Hospitalier Universitaire de Quebec, SaintFoy, QC, Canada,
13 Dana-Farber Cancer Institute, Department of Data Science, Boston, MA, United
States,
14 Charles-Bruneau Cancer Center, CHU Ste-Justine, University of Montreal, Division of Pediatric Hematology-Oncology, Montreal, QC, Canada,
15 UT Southwestern Medical Center, Department of Pediatrics, Dallas, TX, United States,
16 Hasbro Children’s Hospital/Brown University, Division of Pediatric Hematology Oncology, Providence, RI, United States,
17 Harvard Medical School, Department of Pediatrics, Boston, MA, United States
Abstract Body, Introduction:
Over 90% of children with acute lymphoblastic leukemia (ALL) will survive their cancer in the context of >2 years of multi-agent chemotherapy. This intensive treatment paradigm may lead to significant treatment-related financial toxicity for families— an outcome highly relevant to long-term child and family well-being. The magnitude and trajectories of financial toxicity are unknown in pediatric oncology, and necessary to inform optimal screening and intervention strategies for children with cancer and their families. Development of new household material hardship ([HMH], housing, food, or utility insecurity) or income loss during cancer treatment are concrete, targetable metrics of financial toxicity.
We present results from Dana-Farber Cancer Institute (DFCI) ALL Consortium Trial 16-001, the first pediatric oncology clinical trial to systematically collect longitudinal HMH and household income data as an embedded correlative trial aim.
Methods:
DFCI 16-001 (NCT03020030) enrolled children ages 1-<22 years withde novo B- or T-cell ALL at 8 US and Canadian centers from 2017-2021. Participants <18 years were eligible to opt-in to the correlative HMH study at time of initial trial consent. Parents/guardians of participants completed surveys within 32-days of trial enrollment and longitudinally at 6-, 12-, and 24-months. Financial toxicity was the primary endpoint of interest for this secondary analysis, defined by two variables: (1) development of any new HMH domain (food, housing, or utility insecurity) at 6-24 months as compared to baseline and (2) catastrophic income loss defined as ≥25% annual household income loss at 6-24 months compared to baseline. Cumulative incidence of new HMH and catastrophic income loss in the presence of competing risks of coming off study (off-protocol therapy, death, relapse) were estimated using the Aalen-Johansen method. A subcohort analysis was conducted among participants who reported no HMH at baseline. Multivariable competing risk models evaluated the association of patient, household, and disease characteristics with risk of developing new HMH.
Results:
Among 422 participants (15% Hispanic and 7% non-Hispanic Black, 23% single-parent household, 40% annual household income <200% federal poverty level) with evaluable baseline survey data, 115 (27%) reported HMH at baseline. The cumulative incidence of any new HMH was 19.3% (95% CI: 15.9-23.5) at 6-months, 27.7% (95% CI: 23.8-32.4) at 12-months, and 30.0% (95% CI: 25.9-34.7) at 24-months. The cumulative incidence of catastrophic income loss was 20.3% (95% CI: 16.7-24.7) at 6-months, 28.6% (95% CI: 24.5-33.5) at 12-months, and 31.5% (95% CI: 27.2-36.5) at 24-months. Among the subcohort of 307 families with no baseline HMH, the cumulative incidences of any new HMH or catastrophic income loss at 24-months were 24.3% (95% CI: 19.9-29.6) and 27.9% (95% CI: 23.1-33.7), respectively. In multivariable modeling, children who identified as non-Hispanic Black (RR 3.5, 95% CI: 1.7-7.3), lived in a single-parent household (RR 2.1, 95% CI: 1.3-3.2), preferred a non-dominant language (i.e. non-English for US participants and non-English/French for Canadian participants, RR 2.1, 95% CI: 1.2-3.6), or had baseline household income <200% federal poverty level (RR 1.8, 95% CI: 1.1-2.9) were more likely to develop new HMH during treatment.
Conclusion:
Nearly a third of families of children receiving chemotherapy for ALL develop catastrophic financial toxicity during therapy including new unmet basic needs such as food insecurity, or ≥25% income loss. A majority experience this financial toxicity by 6-months into treatment, identifying a key inflection point for potential intervention. Importantly, nearly 1 in 4 families who had no HMH at the time of their child’s diagnosis developed HMH during therapy. These findings stress the clinical importance of longitudinal financial screening over the course of cancer treatment, given the high prevalence of new material needs that arise and the potential to address these needs with family-centered interventions. Future work will assess the impact of early financial toxicity on clinical outcomes in this population and focus on the development of interventions to mitigate the profound financial toxicity impacting families during leukemia care.
Keywords:
Clinical Trials, Lymphoid Malignancies, Supportive Care, Human, Study Population, Health Disparities Research, Lymphoid Leukemias, Health Economics, Patient-Reported Outcomes, Diseases, Clinical Research, ALL, Research, Treatment Considerations, Pediatric, Clinical Practice (Health Services And Quality)