Disability support provider concerned about payment pause during Medicaid audit
Description
Leaders of programs for mental health, in-home care supports, medical transportation and a variety of senior care services are reeling from Gov. Tim Walz’s announcement Wednesday that their payments will be stopped for up to 90 days.
That's to give time for a third-party firm, Optum, to conduct an audit of their billing for Medicaid services in an effort to root out fraud.
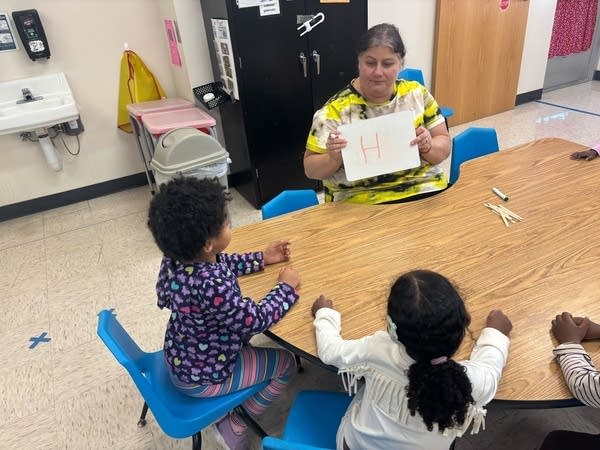
The governor’s plan also freezes money for PCAs, or personal care assistants. Sue Schettle, the CEO of ARRM, which oversees in-home and community-based care for Minnesotans with disabilities, joined MPR News host Cathy Wurzer to talk about what that means for providers, patients and care institutions.
The following transcript has been lightly edited for clarity. Listen to the conversation by clicking the player button above.
Did groups like yours get a heads-up from the governor’s office about the audit and payment pause?
No, we found out about it about the same time that the general public did. We’ve had a long-standing relationship with the Minnesota Department of Human Services and the governor's office, and so we were really surprised that this came out in the way that it did. It just really hit with a thud.
We had a lot of providers who were just questioning: What does this mean? When does it go into effect? How are we going to operate if the payments are frozen for 30, 60, 90 days? And so it was really quite surprising, and it really did cause a lot of panic, not only with my members who provide support to people where they live, but it really had a trickle-down effect to the individuals that they support and their families who are concerned about who’s going to be caring for my person. So it really did not roll out well.
- From Minnesota NowProvider: Pausing Medicaid payments for fraud audit would 'decimate' disability services
- To combat fraud,Walz administration adds third-party entity to examine Medicaid billing
- Walz, legislatorscrack down on fraud schemes on two fronts
Can you briefly describe how your providers receive reimbursement from the state?
It’s a fee-for-service setup where providers submit claims once the services have been provided. As I understand it, the way that fraud will be detected is by looking for outliers — things that just don’t look right, that weren’t maybe in the person’s service authorization plan, just something that looks a little wonky — and then they would pause payment.
But our problem was that it was not described early on; it was when the press release came out from the governor's office. It was the implication that this was going to be applicable to all of the 14 services, which impacts a lot of people, and that payment would be held up for all of those until fraud was reviewed. We’re all about detecting fraud and making sure that that doesn’t happen. The way that it was rolled out made us think that it was going to be a sweeping payment stop. But we’ve come to realize that, with further clarification, it won’t be sweeping; it’ll be just identifying those outliers, which we are supportive of.
However, we don’t know what that criteria look like. Is it, was there an exception that was in the mix here, which would lead to higher payments? There are still a fair number of questions that we have. I'm thankful that Friday morning, we did get a response to our request for a meeting with the Department of Human Services and maybe the governor's office. We’re getting there, but this has really been a very busy week answering lots of questions about things, so I think we can do better.
Walz has been under fire for the amount of fraud seen in various state programs, so he feels that this pause is needed. What’s the atmosphere right now around state funding for programs like yours?
Oh man, it’s rough. People are really afraid. It was rough before the scrutiny. We should root out fraud. We have to figure that out. But providers operate on razor-thin margins. I’ve been at ARRM now for eight years, and I’m always amazed at the creativity and the ways that providers support people when maybe the payments aren’t covering everything. They’re still in this because they care for people with disabilities, but there’s just a lot of uncertainty because of what’s happening here in the state and also at the federal level, just a lot of questions and concern.
If someone has a PCA that comes into their home, will that PCA be paid for the next 30, 60, 90 days or not?
It would depend on the circumstances. If there’s a person who is being supported by a PCA — or in our industry, we call them direct support professionals — and there was something that was flagged by Optum, the payment could stop at that point. And then the provider would have to decide, do we continue the services and not get paid, or do we put in a suspension of services and not support that individual? It really depends on each individual circumstance, but there is a possibility that the person being supported would not be supported anymore.
And then you wonder, well, what does that mean? And how does that person get other support from other providers? And what's the role of DHS in that? Are they going to help plug that person in? Those are the questions we don’t have answers to today.