Episode #7: Continuous Glucose Monitors
Description
In this episode, Hannah and Victoria speak with Angie Alt about the use of continuous glucose monitors in non-diabetic populations.
Angie Alt is a writer, community care activist, independent researcher, and former health coach and nutritional therapist. After a decade of helping clients manage chronic illness through nutrition and lifestyle and training practitioners to utilize the autoimmune protocol in their practices, she shifted her focus from teaching individuals about self-care concepts toward community care-centered work more well-suited to the cooperative and social nature of human well-being. Angie now writes at Notes from a Neighbor, a weekly newsletter on new ways to frame the pressing health and wellness challenges we face collectively and the small, slow, simple actions we can take to respond meaningfully.
2022 article Angie wrote that received some pushback from her audience: https://autoimmunewellness.com/are-wearable-health-trackers-helping-or-harming/
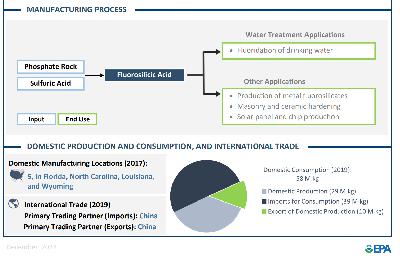
Continuous Glucose Monitoring (CGM) refers to a medical device that measures glucose levels in dermal interstitial fluid. These levels correspond closely with blood glucose concentrations.
History
* https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8120065/
Continuous Glucose Monitoring Devices: Past, Present, and Future Focus on the History and Evolution of Technological Innovation
>> Why CGMs were invented: Traditionally, the principal method of glucose monitoring for people with diabetes has been through self-monitoring of blood glucose (SMBG) without a clear consensus on sampling frequency that varied between four and ten times per day, for insulin-dependent patients with diabetes
1999: First cgm system by Minimed: monitored along with calibration via finger stick every 6-12 hours to monitor over 3 days - info sent straight to healthcare provider
Medtronic Guardian RT and the Dexcom STS—launched in 2005 and 2006 - patient could see results
2007: Dexcom first continuous monitor that recorded for 7 days
2018: Abbott launched the FreeStyle Libre in the United States, the first flash glucose monitoring system
Continuous monitoring allows the user to see trends vs. a finger stick which is just one measurement.
2019: Nutrisense
2024: FDA approves first OTC CGM by Dexcom - intended for those 18 + who don’t require insulin
Pop culture & Influencers:
* https://www.instagram.com/jason.wittrock/ “Fit Dad” whose content is videos of him using his CGM to test isolated foods.
* Nutrisense: CGM available without an rx, pretty popular on social media with wellness influencers https://www.instagram.com/nutrisenseio/
2 weeks $185
3 month membership $300 per month
Evidence
* Review on continuous glucose monitor use in healthy populations: https://www.mdpi.com/1424-8220/22/5/2030
Authors state that "CGM has a high potential for health benefits and self-optimization. More scientific studies are needed to improve the interpretation of CGM data. The interaction with other wearables and combined data collection and analysis in one single device would contribute to developing more precise recommendations for users."
But one author is on the Abbott Advisory Board. Along with Ensure and Pedialyte, they also make...drumroll please...CGMs. https://www.abbott.com/consumer.html#diabetes-care
* https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10460390/
Authors state that "The inter-day reproducibility of the CGM results was greater for subjects with diabetes (ICC 0.46 [CI 0.39–0.55]) than for normoglycaemic subjects (ICC 0.30 [CI 0.27–0.33]); the value for prediabetic subjects was intermediate (ICC 0.37 [CI 0.31–0.42]). For normoglycaemic subjects, inter-day reproducibility was poorer among the younger (ICC 0.26 [CI 0.21–0.30]) than the older subjects (ICC 0.39 [CI 0.32–0.45]).
>> Inter-day reproducibility was poorest among normoglycaemic subjects, especially younger normoglycaemic subjects, suggesting the need to monitor some patient groups more often than others." <<
* https://www.sciencedirect.com/science/article/pii/S0026049523002445
Continuous glucose monitoring in a healthy population: understanding the post-prandial glycemic response in individuals without diabetes mellitus
“There has been a recent trend among individuals without diabetes using these devices as a means of monitoring their health. The increased visibility of glucose data has allowed users to study the effect lifestyle has upon post-prandial glucose levels. Although post-prandial hyperglycemia is well understood in the setting of diabetes, its impact in individuals without diabetes is less well defined. This article reviews the factors which contribute to post-prandial hyperglycemia in individuals without diabetes and how the data obtained from continuous glucose monitoring can be used to improve an individual's metabolic health.”
PPHG is defined as a sharp rise in plasma glucose concentrations following food intake and is influenced by many factors including the timing, quantity and composition of a consumed meal [3].
* CHO content, complex CHO, protein composition of meals
* Glycemic index of CHO foods
* Meal timing
* Hypothalamus, circadian timing
*In metabolically healthy individuals, the glucose curve tends to be biphasic, defined as a curve that shows a peak around 30–60 min after a meal, which then decreases but is followed by another elevation 90–120 min after the meal. A biphasic curve is metabolically preferable over a monophasic curve.
* Gut microbiome
* hormonal status
* stress/cortisol levels
* metabolic health
* intercurrent illness
* Exercise
* Genetic variation
* Age
* BMI
* Pre-peri-postmenopause in females
* Sleep timing/quality/duration
* AM dopamine action/sympathetic tone
* Smoking
* Rx meds: β-blockers, thiazide diuretics, corticosteroids, and statins
* Caffeine
Other pubs show:
* Vitamin C
* Various micronutrients
“Based on the published evidence, we suggest most adults could potentially benefit from wearing a CGM, at least for a two-to-four-week period, to better understand their glucotype and recognise how different foods affect their own glycemic response.
In addition to reducing the long-term risk of cardiovascular disease such as coronary artery disease and stroke, there is evidence to support controlling post-prandial glucose excursions for weight loss, optimized mental health, suppressed hunger, and improved sleep.”
* A large number of people with prediabetes are undiagnosed - up to 40%?https://health.gov/healthypeople/objectives-and-data/browse-objectives/diabetes/reduce-proportion-adults-who-dont-know-they-have-prediabetes-d-02
* Postprandial glucose ranges: https://diabetesjournals.org/care/article/24/4/775/23438/Postprandial-Blood-Glucose
* Non-diabetic: 140 or < ~1 hour after the start of the meal, return to normal levels 2-3 hours after eating
* Diabetic: Peak insulin is delayed, so 2 h after the start of a meal is practical, generally approximates the peak value in patients with diabetes, and provides a reasonable assessment of postprandial hyperglycemia. Specific clinical conditions, such as gestational diabetes or pregnancy complicated by diabetes, may benefit from testing 1 h after the meal
“The host response to any respective glucose sensor will define sensor sensitivity, sensor performance, and ultimately sensor longevity. As such, one significant limitation of all implantable glucose monitoring devices is the foreign body response (FBR), which is an inflammatory reaction stimulated by the host’s immune system in response to a foreign substance. An FBR commences when macrophages, particularly pro-inflammatory M1 macrophages, are recruited to the sensor site through the skin’s vas