My Gum Graft, My Third Child: What Perimenopause Did to My Mouth
Description
Content warning: if you experience fear of the dentist, please take care when reading.
TL;DR*
Fluctuating/reduced estrogen in perimenopause can mean bone density reduces in jaws, jaw changes, exposed teeth/receding gums leave us vulnerable to loosening/losing teeth.
Prevention is definitely better than cure, especially in the case of periodontal disease.
Avoid over brushing and under brushing.
The Goldilocks Effect may just help you avoid a gum graft.
*Guess what? I have no dentistry training, but my friend Dr Kate O’Hara, a retired dentist, has co-written the sciencey bit with me.
This post also includes links to sources should you wish to read what experts have to say on this topic.
Arriving home with a fresh, raw gum graft, having paid a fortune for the privilege, one traumatic day almost six years ago was harrowing. Fittingly, it was Halloween. My husband pulled up on the driveway, our two sons and I his passengers, returning home from Wellington late one Thursday afternoon.
In the front passenger seat, I had winced all the way home. By the time we made it 50km North up the Kāpiti Coast Centennial Highway, I was mute, silenced by surgery. Eyes wet with tears, my usual compulsive comfort eating was now out of reach. Water and smooth soups were all that was on the menu, but they would not provide the dopamine I needed in an effort to self-medicate.
It felt every bit like I was arriving home with a newborn baby, after having undergone the prolonged procedure, getting stitched back up, and nursing a tender vulnerable new existence.
My tender palate had been harvested for a wedge of soft inner tissue that was then sutured in place, attaching it over the exposed roots of my lower front teeth.
Believe it or not, it was exponentially more unpleasant than it sounds.
It took all my self-restraint to keep my tongue out of the wound so as not to disturb the sutures and compromise the attachment of the gum graft, which would have caused further bleeding and rendered the surgery pointless.
I was under strict instructions from my periodontal surgeon to seek immediate medical help should I experience any unmanageable pain, fever or blood loss. Hygienic maintenance of the site was my number one priority, in order to prevent infection.
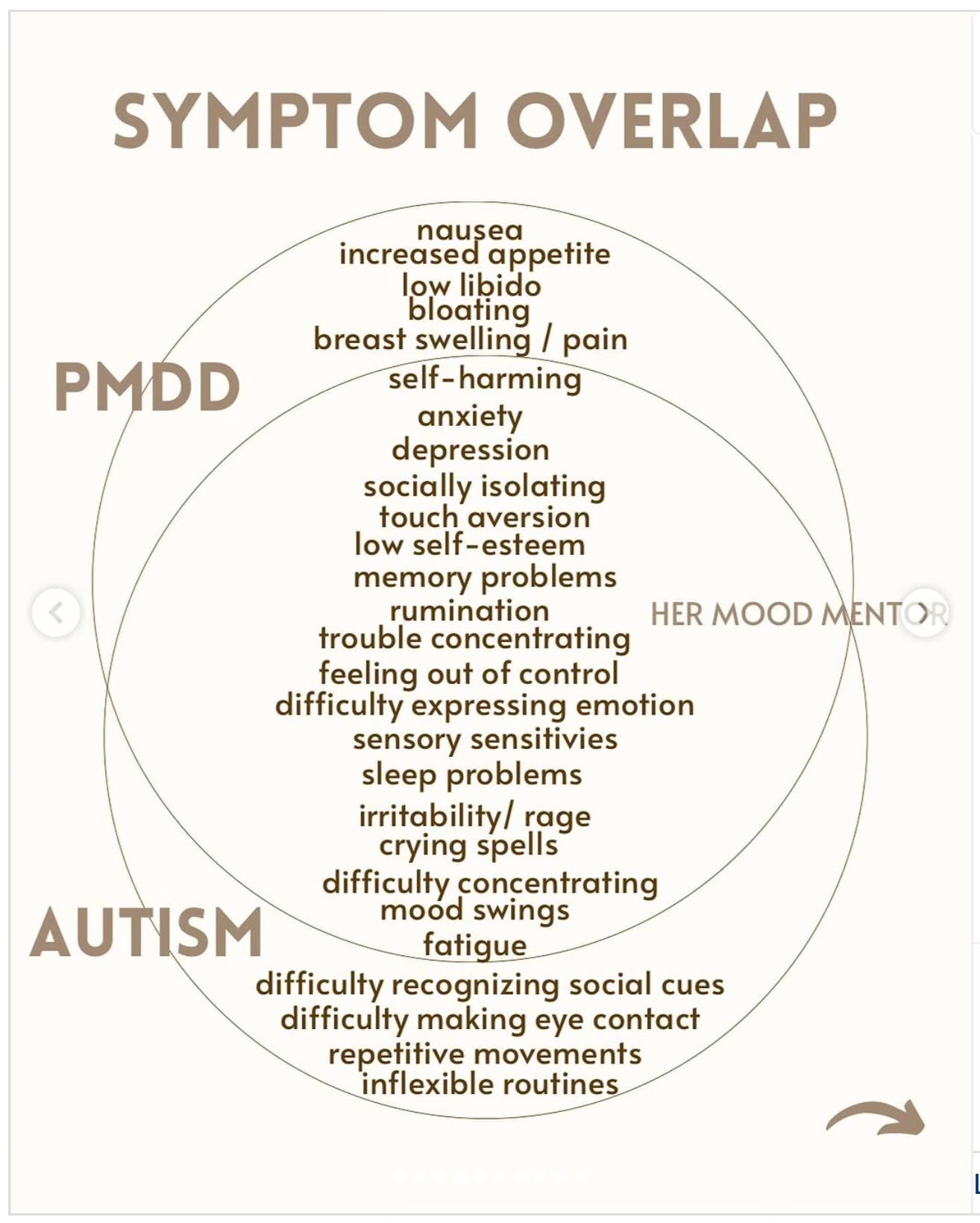
In hindsight, as is the case with my most distressing ailments of late, periodontal disease was probably due to the culmination of decades of undiagnosed neurodivergence and undetected early perimenopause.
It was a lot to deal with, and I will spare you all the gory details. In telling you this though, I would also love to save you from requiring such a procedure by explaining what led me to the periodontist’s chair back in October 2019, aged 38.
With any luck, you haven’t previously heard about or experienced periodontal disease. I certainly wish I hadn’t.
What is periodontal disease?
Please note: The following description has been co-written with the help of Dr Kate O’Hara, late-diagnosed neurodivergent woman, perimenopausal, qualified and retired dentist.
Her explanations are italicised below. I would like to thank her for her help, I was feeling out of my depth with this section! Not to mention a little triggered by revisiting this upsetting time of my life.
Periodontal disease is a severe form of gum disease. It is what happens to some people’s gums when more common gum disease (gingivitis) symptoms go untreated, but not in everybody.
Your risk of developing periodontal disease increases with factors such as:
* Genetics i.e. a family history of the condition
* Poor oral hygiene
* Smoking
* Systemic diseases e.g. diabetes
* Stress and hormonal changes
What I wish I’d understood decades ago is that plaque builds up on teeth overnight. Dental plaque is made up of bacteria, saliva, food particles and (so I have been told) dead sloughed skin from inside our cheeks. Unlike the rest of the dry skin on our bodies, it cannot flake and fall off, instead it mixes with saliva and gets trapped in the gumline.
Cleaning teeth thoroughly twice daily gives us two chances to remove plaque by flossing and brushing teeth before it forms tartar, also known by dentists as calculus.
Any remaining plaque can harden - everyone produces tartar (calculus) but at different rates, and based on factors such as:
* Saliva composition and flow
* Poor oral hygiene
* Smoking
* Diet
* Tooth crowding
* Having fixed retainers can make cleaning more difficult especially behind the lower anterior (front) teeth.
* What types of bacteria colonise your mouth - some people carry more of the periodontal disease causing bacteria than others.
If left unbrushed and unflossed (or brushed/flossed sub-optimally) for 24-72 hours, remaining plaque may harden and become tartar that cannot easily be removed, except by a dentist or dental hygienist. The tartar can cause gaps to form between teeth and gums, under the visible gumline. This may lead to gum recession and thinning - coming away from the tooth, exposing sensitive dental roots, leaving them vulnerable to decay, and bone loss in the jaw.
This bone loss needs preventing in order to reduce the chance of later tooth loss.
These severe gum recessions are called periodontal pockets. The pockets are measured by a dentist and, at a certain measurement, may lead to a referral to a periodontist (a gum specialist).
The periodontist will assess the condition and carry out more in depth treatment which may include surgical or non-surgical deep root cleaning and gum grafting. In most cases once the condition is under control they will refer you back to your dentist and or hygienist for ongoing monitoring and maintenance.
I don’t want to upset anyone, nor retraumatise myself, by describing the procedure in any further detail.
Here is an external link to a a basic description of the procedure, including benefits and risks of periodontal surgery.
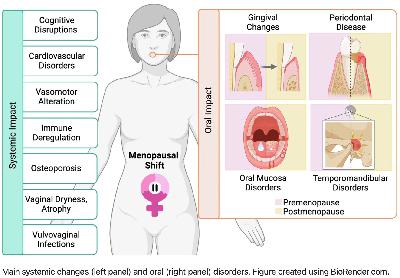
What are the common dental and oral symptoms of perimenopause?
To contextualise periodontitis as a severe and fortunately rarer gum disease, let’s firstly list what we can expect as more likely, and less risky, symptoms that can occur during the menopause transition:
* Gum and tooth sensitivity
* Bleeding gums
* Dry mouth
* Burning mouth
* Altered taste
* Skin thinning of gums and palate
* Grinding and clenching teeth (associated with anxiety, may only occur during sleep)
* Overall reduction in bone mass density, which can occur in the jawbones occasionally leading to loose and lost teeth
More information here:
Unraveling the Connection: Menopause, Peri-Menopause and Periodontal Health (Pure Periodontics)
Hormone Replacement Therapy shown to be highly effective in reducing gum disease (Oral Health Foundation)
How Menopause Affects Your Oral Health (Healthline)
Menopause and the microbiome
There is still so little known about the inner workings of women and AFABs, because history has attributed our non-male biology, anatomy and menstrual cycles to witchcraft and hysteria.
The human microbiome, not to mention all research into female bodily systems, have been scientifically explored less than outer space, which I find out of this world.
Fortunately there is now a growing research interest into the role of the female intestinal (gut) microbiome, the oral microbiome, and the role that fluctuating hormones play in the menopause transition and beyond.
Menopausal shift on women’s health and microbial niches (Nieto, M. et al., 2025) highlights that, during the perimenopausal transition, fluctuating hormone levels impact the microbiome. The changes to the microbiome communities leads to oral, intestinal (gut) and urogenital health complications and makes us susceptible to disease.
‘The gradual decline in hormone levels during perimenopause disrupts the balance of the microbiome, leading to a variety of anatomical conditions and health complications…
‘… Estrogen influences microbial communities while microbes can metabolize and influence estrogen levels. Thus, the interaction between hormones and the microbiome is complex and bidirectional. Understanding the menopausal shift encompasses how hormonal changes, environmental factors, and microbial dynamics affect menopausal symptoms and women’s health.’
Source: Maria R. Nieto, Maria J. Rus, Victoria Areal-Quecuty, Daniel M. Lubián-López & Aurea Simon-Soro, <a hr