Understanding Swelling and Scar Tissue After Knee Replacement
Description
An Interview with Lisa Alarcon, Director of Physical Therapy
Understanding Swelling and Scar Tissue After Knee Replacement
The composition of the swelling that occurs in the knee depends on how long it’s been there. The longer the swelling is in the knee the more likely you will have to deal with stiffness. If you’ve ever noticed you can push on someone’s skin and it stays ‘dipped’, those patients have a lot more protein in that fluid. And so what happens as you get that fluid in the knee structure that supports it (the joint capsule,) it swells like a balloon. Swelling and scar tissue after knee replacement are the two biggest challenges you will face.
So the more swelling that’s in that knee, the tighter the balloon gets. Once that balloon gets too tight, you have a significant limit in how much you can move your knee. When that happens, you don’t move your knee because it hurts, it’s uncomfortable, so you keep it still. Keeping it still only creates kind of this vicious cycle. Now it doesn’t move, so you can have scar tissue start to set up.
<figure class="wpb_wrapper vc_figure">

</figure>
Anytime you put your body in a certain comfortable position and then you start to move out of that position, everything’s like, oh wait a minute, that doesn’t feel so good. And that’s also what’s happening in a fresh knee joint, especially immediately following surgery. Those structures are not happy that they’ve been disturbed. They like to be where they are. They don’t want to be cut, and that has all happened with the surgery. The body’s natural system says, “I’m going to limit how much motion I want this knee to have, and so I’m going to send the swelling in.”
Fibrosis
Fibrosis is another way to look at scar tissue. It’s ‘scar tissue plus.’ You can kind of think of the tissue surrounding the knee like spider webs. And so we can move the knee joint a little bit, or the shoulder, or whatever joint it happens to be, and we can break those spider webs, and we can get some range of motion back.
With fibrosis the tissue is more like duct taping the joint. The components that make up something that’s fibrotic versus something that’s strict scar tissue is that the tissue is a little bit more intense. The tissue is stronger, the tensile strength is stronger. It’s thicker. So fibrosis compared to kind of what I would consider normal scar tissue is just really kind of ‘scar tissue on steroids,’ and it’s a lot harder to break through. Usually those with this thicker scar tissue are the people that need the Manipulation Under Anesthesia (see: Julie Avoids an MUA) because they’ve had that fibrotic tissue start to set in, and so that’s the difference really between kind of general scar tissue and something that’s gone fibrotic.
You may have seen people that have those really big, bumpy kind of gnarly looking scars. Those patients are more likely to have that same kind of body response on the inside. Fibrosis depends on genetics, it depends on how long you want to sit still for, it depends on things like: ‘I had a knee replacement, and then I had an injection, and then I had another knee replacement.’ So if you have some or all of these other factors, that limit your ability to move that joint, you’re going to get that fibrosis a lot faster. And so the ‘when and the why’ of fibrosis kind of combine, and based on genetics and these other extenuating circumstances recovery can be more challenging. Certainly the less you move the knee, the less frequently you move the knee, the more likely you are to build in that kind of block, and it really feels like a block.
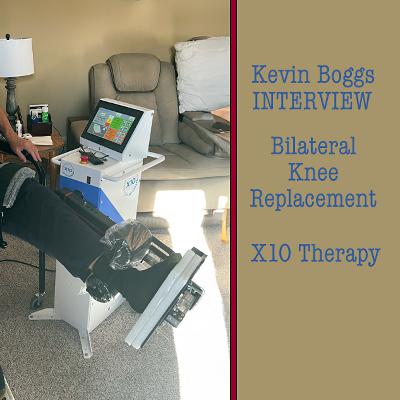
The X10 Knee Recovery System™
I think the X10 helps prevent scar tissue in general. If we can prevent general scar tissue, we certainly can prevent scar tissue on steroids, when you talk about something like a fibrosis, because you get in and you get moving early. We’ve had physicians who love the progress of their patients so much, they don’t want to put the CPM in the hospital, they want to bring X10 into the hospital, okay? And that’s amazing, to take someone who’s an orthopedic surgeon who’s been an orthopedic surgeon for a long time, who’s relied on the CPM for a long time and have them say, “I don’t want to do that anymore. I like the X10. I like how it works so much, I’m going do it even sooner. I want that patient on the X10 the hour after they come out of surgery or in those kinds of parameters.”
And so X10 as far as preventing fibrosis I think is absolutely what it does. But beyond that, I think if you have a patient that has fibrosis in their knee, or has some kind of a contracture, you can also bring X10 in in that situation, because of the ability to alter the hold times on the machine. On the X10 you can hold in a challenging but not painful position for three seconds, or for longer than that. With the fibrotic joint, I just need to hold longer. So even if a joint is fibrotic, we may not have to worry about a manipulation.
In those situations, whether it’s preventing the fibrosis or taking the fibrosis and trying to kind of break through it and get some more stretch