ADHD and Co-Occurring Conditions: Anxiety, Mood, and Learning Disorders
Description
Welcome or welcome back to Authentically ADHD, the podcast where we embrace the chaos and magic of the ADHD brain. Im carmen and today we're diving into a topic that's as complex as my filing system (which is to say, very): ADHD and its common co-occurring mood and learning disorders. Fasten your seatbelts (and if you're like me, try not to get distracted by the shiny window view) – we're talking anxiety, depression, OCD, dyslexia, dyscalculia, and bipolar disorder, all hanging out with ADHD.
Why cover this? Because ADHD rarely rides solo. In fact, research compiled by Dr. Russell Barkley finds that over 80% of children and adults with ADHD have at least one other psychiatric disorder, and more than half have two or more coexisting conditions. Two-thirds of folks with ADHD have at least one coexisting condition, and often the classic ADHD symptoms (you know, fidgeting, daydreaming, “Did I leave the stove on?” moments) can overshadow those other disorders. It’s like ADHD is the friend who talks so loud at the party that you don't notice the quieter buddies (like anxiety or dyslexia) tagging along in the background.
But we’re going to notice them today. With a blend of humor, sass, and solid neuroscience (yes, we can be funny and scientific – ask me how I know!), we’ll explore how each of these conditions shows up alongside ADHD. We’ll talk about how they can be misdiagnosed or missed entirely, and—most importantly—we’ll dish out strategies to tell them apart and tackle both. Knowledge is power and self-awareness is the key, especially when it comes to untangling ADHD’s web of quirks and comrades in chaos. So, let’s get into it!
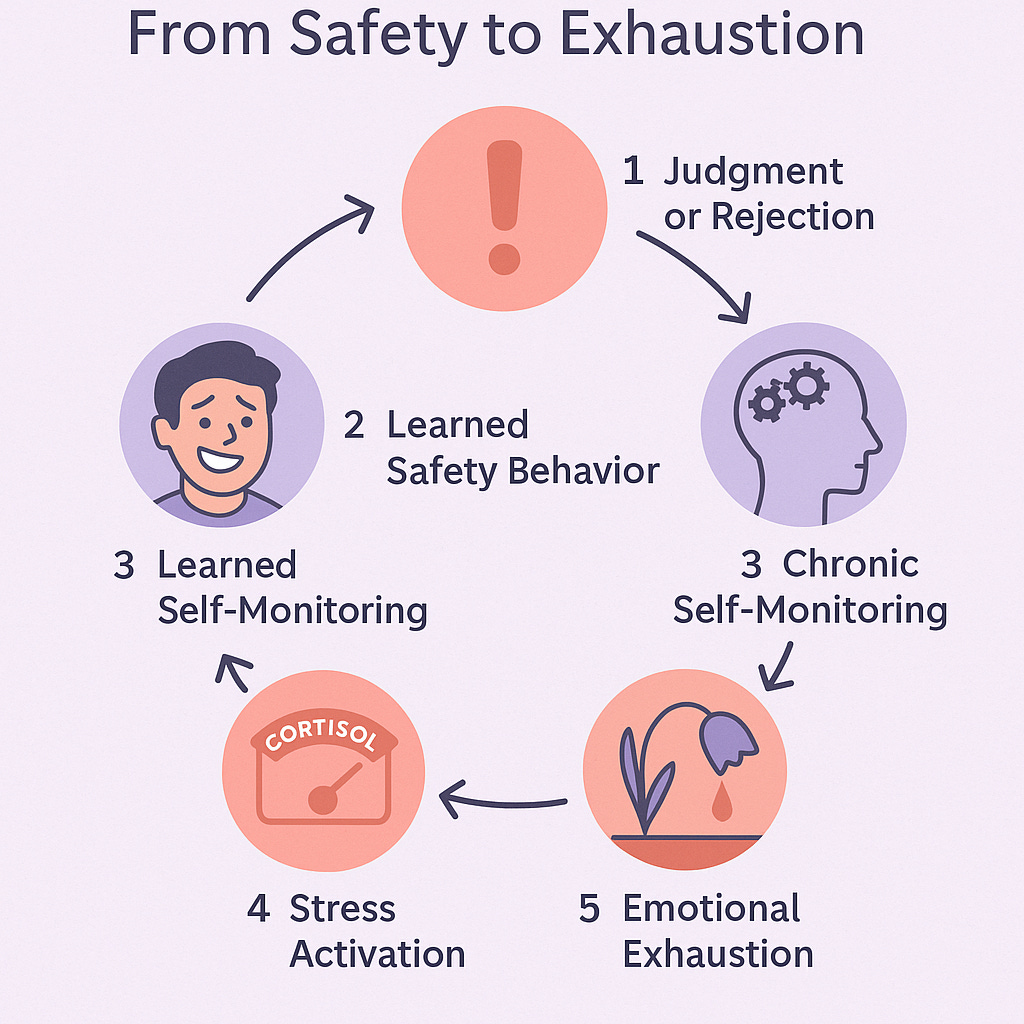
ADHD and Anxiety: Double Trouble in Overdrive
Let’s start with anxiety, ADHD’s frequent (and frantic) companion. Ever had your brain ping-pong between “I can’t focus on this work” and “I’m so worried I’ll mess it up”? That’s ADHD and anxiety playing tango in your head. It’s a double whammy: ADHD makes it hard to concentrate, and anxiety cranks up the worry about consequences. As one study notes, about 2 in 5 children with ADHD have significant problems with anxiety, and over half of adults with ADHD do as well. In other words, if you have ADHD and feel like a nervous wreck half the time, you’re not alone – you’re in very good (and jittery) company.
ADHD and anxiety can look a lot alike on the surface. Both can make you restless, unfocused, and irritable. I mean, is it ADHD distractibility or am I just too busy worrying about everything to pay attention? (Hint: it can be both.) Especially for women, ADHD is often overlooked and mislabeled as anxiety. Picture a girl who can’t concentrate in class: if she’s constantly daydreaming and fidgety, one teacher calls it ADHD. Another sees a quiet, overwhelmed student and calls it anxiety. Same behavior, different labels. Women in particular have had their ADHD misdiagnosed as anxiety or mood issues for years, partly because anxious females tend to internalize symptoms (less hyperactive, more “worrier”), and that masks the ADHD beneath.
So how do we tell ADHD and anxiety apart? One clue is where the distraction comes from. ADHD is like having 100 TV channels in your brain and someone else is holding the remote – your attention just flips on its own. Anxiety, on the other hand, is like one channel stuck on a horror movie; you can’t focus on other things because a worry (or ten) is running on repeat. An adult with ADHD might forget a work deadline because, well, ADHD. An adult with anxiety might miss the deadline because they were paralyzed worrying about being perfect. Both end up missing the deadline (relatable – ask me how I know), but for different reasons.
Neuroscience is starting to unravel this knot. There’s evidence of a genetic link between ADHD and anxiety – the two often run in the family together. In brain studies, both conditions involve irregularities in the prefrontal cortex (the brain’s command center for focus and planning) and the limbic system (emotion center). Essentially, if your brain were a car, ADHD means the brakes (inhibition) are a bit loose, and anxiety means the alarm system is hyper-sensitive. Combine loose brakes with a blaring alarm and you get… well, us. Fun times, right?
Here’s an interesting tidbit: Females with ADHD are more likely to report anxiety than males. Some experts think this is partly due to underdiagnosed ADHD – many girls grew up being told they were just “worrywarts” when in fact ADHD was lurking underneath, making everyday life more overwhelming and thus feeding anxiety. As Dr. Thomas Brown (a top ADHD expert) points out, emotional regulation difficulties (like chronic stress or worry) are characteristic of ADHD, even though they’re not in the official DSM checklist. Our ADHD brains can amplify emotions – so a normal worry for someone else becomes a five-alarm fire for us.
Now, action time: How do we manage this dynamic duo? The first step is getting the right diagnosis. A clinician should untangle whether symptoms like trouble concentrating are from anxiety, ADHD, or both. They might ask: Have you always had concentration issues (pointing to ADHD), or did they start when your anxiety kicked into high gear? Also, consider context – ADHD symptoms occur in most settings (school, work, home), while pure anxiety might spike in specific situations (say, social anxiety in crowds, or panic attacks only under stress).
Treatment has to tackle both. Therapy – especially Cognitive Behavioral Therapy (CBT) – is a rockstar here. CBT can teach you skills to manage worry (hello, deep breathing and logical rebuttals to “what if” thoughts) and also help with ADHD organization hacks (like breaking tasks down, creating routines). Many find that medication is needed for one or both conditions. Stimulant meds (like methylphenidate or amphetamines) treat ADHD, but in someone with severe anxiety, a stimulant alone can sometimes ramp up the jitters. In fact, children (and adults) with ADHD + anxiety often don’t respond as well to ADHD meds unless the anxiety is also addressed. Doctors might add an SSRI or other anti-anxiety medication to the mix, or choose a non-stimulant ADHD med if stimulants prove too anxiety-provoking.
Let me share a quick personal strategy (with a dash of humor): I have ADHD and anxiety, so my brain is basically an internet browser with 50 tabs open – and 10 of them are frozen on a spinning “wheel of doom” (those are the anxieties). One practical tip that helps me distinguish the two is to write down my racing thoughts. If I see worries like “I’ll probably get fired for sending that email typo” dominating the page, I know anxiety is flaring. If the page is blank because I got distracted after one sentence... well, hello ADHD! This silly little exercise helps me decide: do I need to do some calming techniques, or do I need to buckle down and use an ADHD strategy like the Pomodoro method? Try it out: Knowledge is power, and self-awareness is the key.
Quick Tips – ADHD vs Anxiety: When in doubt, ask what’s driving the chaos.
* Content of Thoughts: Racing mind full of specific worries (anxiety) vs. racing mind full of everything except what you want to focus on (ADHD).
* Physical Symptoms: Anxiety often brings friends like sweaty palms, racing heart, and tummy trouble. ADHD’s restlessness isn’t usually accompanied by fear, just boredom or impulsivity.
* Treatment Approaches: For co-occurring cases, consider therapy and possibly a combo of medications. Experts often treat the most impairing symptom first – if panic attacks keep you homebound, address that alongside ADHD. Conversely, untreated ADHD can actually fuel anxiety (ever notice how missing deadlines and forgetfulness make you more anxious? Ask me how I know!). A balanced plan might be, say, stimulant medication + talk therapy for anxiety, or an SSRI combined with ADHD coaching. Work closely with a professional to fine-tune this.
Alright, take a breath (seriously, if you’ve been holding it – breathing is good!). We’ve tackled anxiety; now let’s talk about the dark cloud that can sometimes follow ADHD: depression.
ADHD and Depression: When the Chaos Brings a Cloud
ADHD is often associated with being energetic, spontaneous, even optimistic (“Sure, I can start a new project at 2 AM!”). So why do so many of us also struggle with depression? The reality is, living with unmanaged ADHD can be tough. Imagine years of what Dr. Russell Barkley calls “developmental delay” in executive function – always feeling one step behind in managing life, despite trying so hard. It’s no surprise that about 1 in 5 kids with ADHD also has a diagnosable depression, and studies show anywhere from 8% to 55% of adults with ADHD have experienced a depressive disorder in their lifetime. (Yes, that range is huge – it depends how you define “depression” – but even on the low end it’s a lot.) Dr. Barkley himself notes that roughly 25% of people with ADHD will develop significant depression by adulthood. In short, ADHD can come with a case of the blues (not