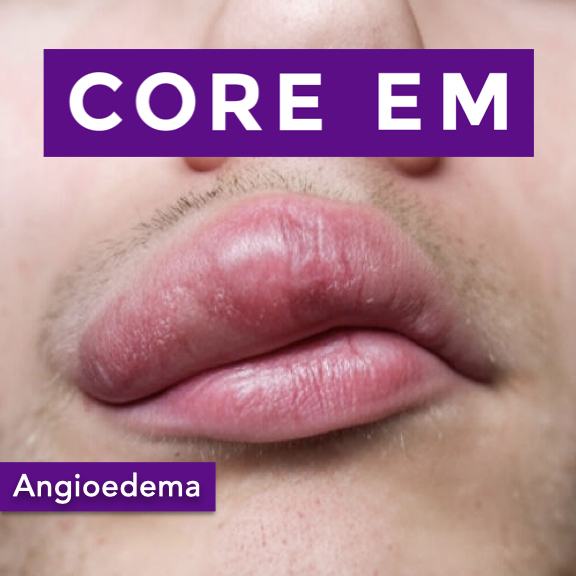
Episode 212: Angioedema
Update: 2025-08-02 1
1
Description
Angioedema – Recognition and Management in the ED
Hosts:
Maria Mulligan-Buckmiller, MD
Brian Gilberti, MD
Download
Leave a Comment
Tags: Airway
Show Notes
Definition & Pathophysiology
Angioedema = localized swelling of mucous membranes and subcutaneous tissues due to increased vascular permeability.
Triggers increased vascular permeability → fluid shifts into tissues.
Etiologies
- Histamine-mediated (anaphylaxis)
- Associated with urticaria/hives, pruritus, and redness.
- Triggered by allergens (foods, insect stings, medications).
- Rapid onset (minutes to hours).
- Bradykinin-mediated
- Hereditary angioedema (HAE): C1 esterase inhibitor deficiency (autosomal dominant).
- Acquired angioedema: Associated with B-cell lymphoma, autoimmune disease, MGUS.
- Medication-induced: Most commonly ACE inhibitors; rarely ARBs.
- Typically lacks urticaria and itching.
- Gradual onset, can last days if untreated.
- Idiopathic angioedema
- Unknown cause; diagnosis of exclusion.
Clinical Presentations
- Swelling
- Asymmetric, non-pitting, usually non-painful.
- May involve lips, tongue, face, extremities, GI tract.
- Respiratory compromise
- Upper airway swelling → stridor, dyspnea, sensation of throat closure.
- Airway obstruction is the most feared complication.
- Abdominal manifestations
- Bowel wall angioedema can mimic acute abdomen:
- Nausea, vomiting, diarrhea, severe pain, increased intra-abdominal pressure, possible ischemia.
- Bowel wall angioedema can mimic acute abdomen:
Key Differentiating Features
- Histamine-mediated: rapid onset, hives/itching, resolves quickly with epinephrine, antihistamines, and steroids.
- Bradykinin-mediated: slower onset, lacks urticaria, prolonged duration, less responsive to standard anaphylaxis medications.
Diagnostic Approach in the ED
- Focus on airway (ABCs) and clinical assessment.
- Labs (e.g., C4 level) useful for downstream diagnosis (esp. HAE) but not for acute management.
- Imaging: only if symptoms suggest abdominal involvement or to rule out other causes.
Treatment Strategies
- Airway protection is always priority:
- Early consideration of intubation if worsening obstruction or inability to manage secretions.
- Histamine-mediated (anaphylaxis):
- Epinephrine (IM), antihistamines, corticosteroids.
- Bradykinin-mediated:
- Epinephrine may be tried if unclear etiology (no significant harm, lifesaving if histamine-mediated).
- Targeted therapies:
- Icatibant: bradykinin receptor antagonist.
- Ecallantide: kallikrein inhibitor (less available).
- C1 esterase inhibitor concentrate: replenishes deficient protein.
- Fresh frozen plasma (FFP): contains C1 esterase inhibitor.
- Tranexamic acid (TXA): off-label, less evidence, considered if no other options.
Complications to Watch For
- Airway compromise: rapid deterioration possible.
- Abdominal compartment syndrome from bowel edema (rare, surgical emergency).
Take-Home Points
- Secure the airway if in doubt.
- Differentiate histamine-mediated vs bradykinin-mediated by presence/absence of hives/itching and speed of onset.
- Use epinephrine promptly if suspecting histamine-mediated angioedema or if uncertain.
- Consider bradykinin-targeted therapies for confirmed hereditary, acquired, or ACE-inhibitor–related angioedema.
- Recognize ACE inhibitors as the most frequent medication trigger; ARBs rarely cause it.
- Labs and imaging generally don’t change initial ED management but aid diagnosis for follow-up care.
Read More
Comments
In Channel