Chapter Fifteen, part 1: Clinical Use of Diuretics
Description
Outline Chapter 15 — Clinical Use of Diuretics
- Among most commonly used drugs
- Block NaCl reabsorption at different sites along the nephron
- The ability to induce negative balance has made them useful in multiple diseases
- Edematous states
- Hypertension
- Mechanism of action
- Three major classes
- Loop
- NaK2Cl
- Up to 25% of filtered sodium excreted
- Thiazide
- NCC
- Up to 3-5% of filtered sodium excreted
- Potassium sparing
- ENaC
- Up to 1-2% of filtered sodium excreted
- Each segment has a unique sodium channel to allow tubular sodium to flow down a concentration gradient into the cell
- Table 15-1 is interesting
- Most of the sodium 55-655 is reabsorbed in the proximal tubule
- Proximal diuretics would be highly effective if it wasn’t for the loop and other distal sites of Na absorption
- Loop Diuretics
- Furosemide
- Bumetanide
- Torsemide
- Ethacrynic acid
- NaK2Cl activated when all four sites are occupied
- Loop diuretic fits into the chloride slot
- In addition to blocking Na reabsorption results in parallel decrease in calcium resorption
- Increase in stones and nephro albinos is especially premature infants which can increase calcium excretion 10-fold
- Thiazide
- Even though they are less potent than loops they are great for hypertension
- “Not a problem in uncomplicated hypertension where marked fluid loss is neither necessary nor desirable”
- Some chlorothiazide and metolazone also inhibit carbonic anhydrase in the proximal tubule
- Increase Calcium absorption. Mentions that potassium sparing diuretics do this also
- Potassium sparing diuretics
- Amiloride
- Spironolactone
- Triamterene
- Act at principal cells in the cortical collecting tubule,
- Block aldosterone sensitive Na channels.
- Discusses the difference between amiloride and triamterene and spiro
- Mentions that trimethoprim can have a similar effect
- Spiro is surprisingly effective in cirrhosis and ascites
- Talks about amiloride helping in lithium toxicity
- Partially reverse and prevent NDI from lithium
- Trial Terence as nephrotoxin?
- Causes crystaluria and casts
- These crystals are pH independent
- Faintly radio opaque
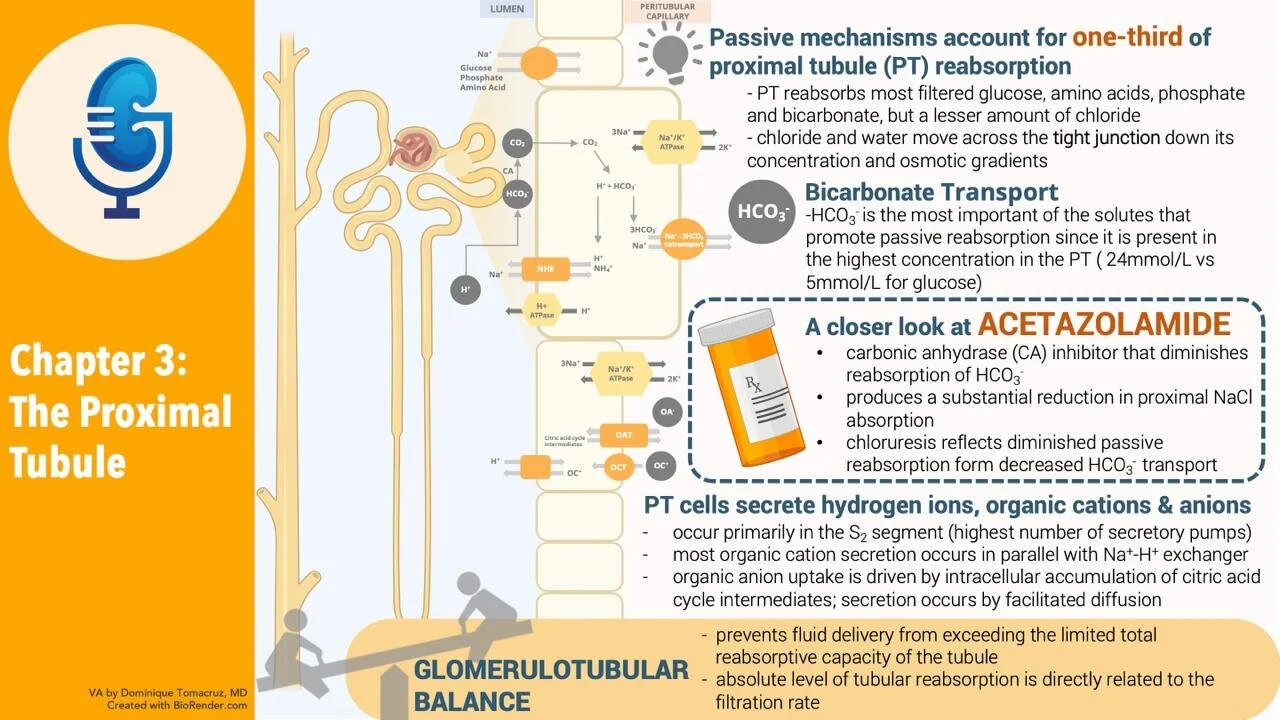
- Acetazolamide
- Blocks carbonic anhydrase
- Causes both NaCl and NaHCO3 loss
- Modest diuresis de to distal sodium reclamation
- Mannitol
- Nonreabsorbable polysaccharide
- Acts mostly in proximal tubule and Loop of Henle
- Causes water diuresis
- Was used to prevent ATN
- Can cause hyperosmolality directly and through the increased water loss
- This hyperosmolality will be associated with osmotic movement of water from cells resulting in hyponatremia, like in hyperglycemia.
- Docs must treat the hyperosmolality not the hyponatremia
- Time course of Diuresis
- Efficacy of a diuretic related to
- Site of action
- Dietary sodium action
- 15-1 shows patient with good short diuretic response but other times of low urine Na resulting in no 24 hour net sodium excretion.
- Low sodium diets work with diuretics to minimize degree of sodium retension while diuretic not working
- Also minimizes potassium losses
- Increase frequency
- Increase dose
- What causes compensatory anti-diuresis
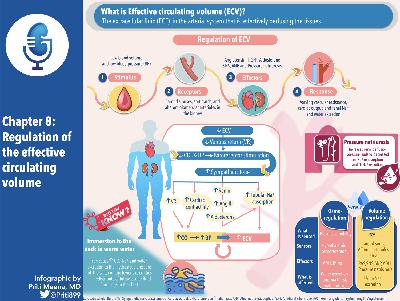
- Activation of RAAS and SNS
- ANG II, aldo, norepi all promote Na reabsorption
- But even when prazosin to block alpha sympathetic and capto[pril to block RAAS sodium retention occurs
- Decrease in BP retains sodium with reverse pressure natriuresis
- Even with effective diuresis there is reestablishment of a new steady state
- Diuresis is countered by
- Increases in tubular reabsorption at non-diuretic sensitive sites (neurohormonal mediated)
- Flow mediated in creases in Tubular reabsorption distal to the diuretic from increased sodium delivery.
- Hypertrophy
- Increased Na-K-ATPase activity
- Decreased tubular secretion of diuretic if renal perfusion is impaired
- Getting to steady state requires
- Diuretic dose and sodium intake be constant
- Sodium balance is reestablished with 3 days of a fixed diuretic dose
- K balance in 6-9 days
- Figure 15-2
- Which means that people on stable doses of diuretics don’t need regular labs, the abnormalities will emerge quickly.
- Maximum diuresis happens with first dose
- Figure 15-3
- Fluid and Electrolyte complications
- Volume depletion
- “Effective circulating volume depletion also can develop in patients who remain edematous. Although fluid persists, there may be a sufficient reduction in intracranial filling pressures and cardiac output to produce a clinically important reduction in tissue perfusion.”
- Azotemia
- Decreased effective circulating volume with diuretic therapy also can diminish renal perfusion and secondarily the GFR.
- Describes the traditional reason for increased BUN:Cr ratio
- Then states that as much as a third of of the rise in BUN may reflect increased urea production; it is possible, for example, that reduced skeletal muscle perfusion leads to enhanced local proteolysis. This increases urea production.
- Hypokalemia
- Loop and thiazide increase urinary potassium losses
- Often lead to hypokalemia
- 50 mg of HCTZ drop K by 0.4 to 0.6 mEq/L with 15% falling below 3.5
- He uses “associated” I think this is a place where we can use cause
- 50 mg of chlorthalidone
- K falls 0.8 to 0.9 mEq/L
- Etiology
- Increased distal delivery of Na and water
- Increased aldo
- From volume depletion
- Underlying disease: cirrhosis and heart failure
- Talk a lot about significance.
- Info sounds dated
- Increased risk of SCD in MRFIT trial
- Association with increased ventricular arrhythmia with hypokalmia
- Increased PVC and complex PVC by 27% with each drop in K of 0.5 mEq/L
- Says that stress can induce epinephrine which can shift potassium inside cells leading to fatal arrhythmia especially if the patient begins at a low potassium concentration
- Says v-fib two fold likely in MI patients with hypokalemia
- Talks about crazy doses of HCTZ and Chlorthalidone 50+mg
- Recommends 12.5 to 15 mg respectively
- Metabolic alkalosis
- Caused by loop and thiazide diuretics
- Two factors cause this
- Increased urinary H loss
- Partly UE to secondary hyperaldo
- Contraction of extracellular volume around remaining bicarb
- Why not contraction hypernatremia, contraction hyperkalemia, etc?
- Aldosterone contributes by stimulate ing H-ATPase
- Stimulating Sodium reabsorption creating lumen negative charge that promotes Hydrogen secretion
- Loop diuretics can also stimulate net H loss by increased Hsecretion in the cortical aspect of the thick limb
- This segment has two luminal entry points for na, the traditional NaK2Cl and Na-H exchanger
- Blocking NaK2Cl with loop diuretic stimulates the Na-H exchanger
- Can use NaCl or acetazolamide to treat
- Metabolic acidosis
- K-sparing diuretics reduce both K and H secretion in the collecting tubule
- Avoid if renal failure or on an ACEi
- Good advice to avoid K supplement with the K sparing diuretic
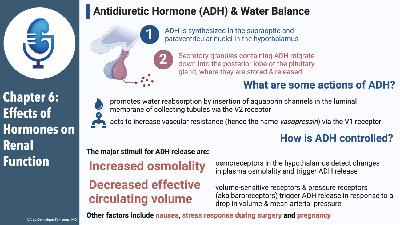
- Hyponatremia
- Diuretics can cause volume depletion leading to enhanced secretion of ADH and to increased water intake
- Almost always due to a thiazide
- Loops destroy the concentrated medullary gradient making ADH less effective
- Hyperdrive is
- Increased urate reabsorption in the proximal tubule
- Process mediated by parallel Na-H and urate OH exchangers see figure 3-13a
- Urate reabsorption varies directly with proximal Na transport and in patients with diuretic-induced volume deficiency both Na and urate excretion are reduced.
- May be related to Ang II
- Do not need to treat the hyperuricemia in asymptomatic patients
- Do not develop urate nephropathy because tubular urateis actually low
- Hypomagnesemia
- Generally mild
- Loop diuretics since most reabsorbed in the loop
- Thiazides don’t affect Mg (why with gitelmans?)
- Hypokalemia may directly inhibit tubular cell mg uptake
- Aldosterone increases Mg excretion, so K sparing diuretics decrease Mg secretion
- Determinants of Diuretic responsiveness
- 2 important determinants of diuretic response
- Site of action
- Presence of counterbalancing antinatriuretic forces
- Ang2
- Aldo
- Low systemic BP
- Adds rate of drug excretion as # 2 and a half
- Almost all diuretics are protein bound
- So not well filtered
- Enter tubule through organic anion and organic cation transporter
- This can limit diuretic effectiveness
- Natriuretic response plateaus at higher rates of diuretic excretion due to complete inhibition of the diuretic target
- This plateau in normal people is 1 mg of bumetanide and 40 mg of furosemide given IV
- Double this for oral furosemide, no adjustment needed for bumetanide
- 15-6
- Refractory edema
- Start with a loop diuretic
- Initial aim is to find the effective single dose
- From the paragraph this is about threshold dosing
- Double ineffective doses until good effect
- Suggests maximum furosemide dose is 200 mg IV and 400 mg oral
- Excess sodium intake
- High sodium diet can work to prevent patients from achieving negative sodium balance.<