Chapter Fourteen, part 1. Hypovolemic States
Description
Outline
Chapter 14
- Hypovolemic States
- Etiology
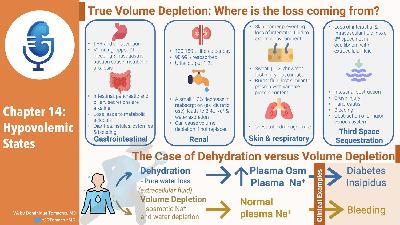
- True volume depletion occurs when fluid is lost from from the extracellular fluid at a rate exceeding intake
- Can come the GI tract
- Lungs
- Urine
- Sequestration in the body in a “third space” that is not in equilibrium with the extracellular fluid.
- When losses occur two responses ameliorate them
- Our intake of Na and fluid is way above basal needs
- This is not the case with anorexia or vomiting
- The kidney responds by minimizing further urinary losses
- This adaptive response is why diuretics do not cause progressive volume depletion
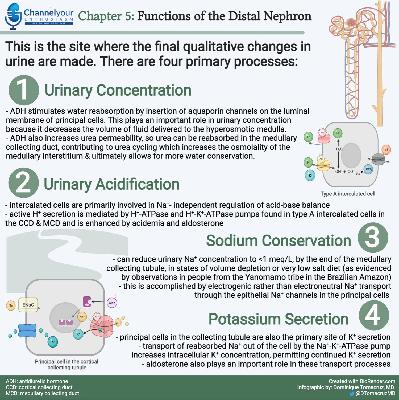
- Initial volume loss stimulates RAAS, and possibly other compensatory mechanisms, resulting increased proximal and collecting tubule Na reabsorption.
- This balances the diuretic effect resulting in a new steady state in 1-2weeks
- New steady state means Na in = Na out
- GI Losses
- Stomach, pancreas, GB, and intestines secretes 3-6 liters a day.
- Almost all is reabsorbed with only loss of 100-200 ml in stool a day
- Volume depletion can result from surgical drainage or failure of reabsorption
- Acid base disturbances with GI losses
- Stomach losses cause metabolic alkalosis
- Intestinal, pancreatic and biliary secretions are alkalotic so losing them causes metabolic acidosis
- Fistulas, laxative abuse, diarrhea, ostomies, tube drainage
- High content of potassium so associated with hypokalemia
- [This is a mistake for stomach losses]
- Bleeding from the GI tract can also cause volume depletion
- No electrolyte disorders from this unless lactic acidosis
- Renal losses
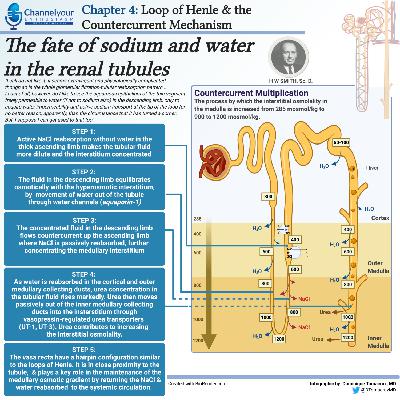
- 130-180 liters filtered every day
- 98-99% reabsorbed
- Urine output of 1-2 liters
- A small 1-2% decrease in reabsorption can lead to 2-4 liter increase in Na and Water excretion
- 4 liters of urine output is the goal of therapeutic diuresis which means a reduction of fluid reabsorption of only 2%
- Diuretics
- Osmotic diuretics
- Severe hyperglycemia can contribute to a fluid deficit of 8-10 Iiters
- CKD with GFR < 25 are poor Na conservers
- Obligate sodium losses of 10 to 40 mEq/day
- Normal people can reduce obligate Na losses down to 5 mEq/day
- Usually not a problem because most people eat way more than 10-40 mEq of Na a day.
- Salt wasting nephropathies
- Water losses of 2 liters a day
- 100 mEq of Na a day
- Tubular and interstitial diseases
- Medullary cystic kidney
- Mechanism
- Increased urea can be an osmotic diuretic
- Damage to tubular epithelium can make it aldo resistant
- Inability to shut off natriuretic hormone (ANP?)
- The decreased nephro number means they need to be able to decrease sodium reabsorption per nephron. This may not be able to be shut down acutely.
- Experiment, salt wasters can stay in balance if sodium intake is slowly decreased. (Think weeks)
- Talks about post obstruction diuresis
- Says it is usually appropriate rather than inappropriate physiology.
- Usually catch up solute and water clearance after releasing obstruction
- Recommends 50-75/hr of half normal saline
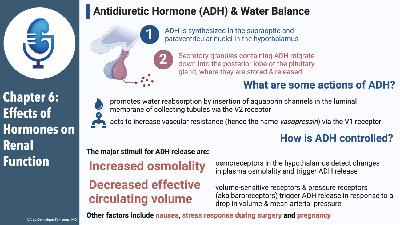
- Talks briefly about DI
- Skin and respiratory losses
- 700-1000 ml of water lost daily by evaporation, insensible losses (not sweat)
- Can rise to 1-2 liters per hour in dry hot climate
- 30-50 mEq/L Na
- Thirst is primary compensation for this
- Sweat sodium losses can result in hypovolemia
- Burns and exudative skin losses changes the nature of fluid losses resulting in fluid losses more similar to plasma with a variable amount of protein
- Bronchorrhea
- Sequestration into a third space
- Volume Deficiency produced by the loss of interstitial and intravascular fluid into a third space that is not in equilibrium with the extracellular fluid.
- Hip fracture 1500-2000 into tissues adjacent to fxr
- Intestinal obstruction, severe pancreatitis, crush injury, bleeding, peritonitis, obstruction of a major venous system
- Difference between 3rd space and cirrhosis ascities
- Rate of accumulation, if the rate is slow enough there is time for renal sodium and water compensation to maintain balance.
- So cirrhotics get edema from salt retension and do not act as hypovolemia
- Hemodynamic response to volume depletion
- Initial volume deficit reduced venous return to heart
- Detected by cardiopulmonary receptors in atria and pulmonary veins leading to sympathetic vasoconstriction in skin and skeletal muscle.
- More marked depletion will result in decreased cardiac output and decrease in BP
- This drop in BP is now detected by carotid and aortic arch baroreceptors resulting in splanchnic and renal circulation vasoconstriction
- This maintains cardiac and cerebral circulation
- Returns BP toward normal
- Increase in BP due to increased venous return
- Increased cardiac contractility and heart rate
- Increased vascular resistance
- Sympathetic tone
- Renin leading to Ang2
- These can compensate for 500 ml